Home » Uncategorized » PVCs: Everything you need to know

Premature Ventricular Contractions (PVCs) are early, extra heartbeats that start in the heart’s lower chambers (the ventricles), disrupting the heart’s normal rhythm for a moment. They are relatively common in 3% to 20% of the general population and are often detected during evaluations for palpitations or incidentally on routine electrocardiograms (ECGs). They often show no symptoms and require no special treatment. But for some, these contractions can cause uncomfortable sensations, and anxiety, or even signal an underlying cardiac problem. Let’s first understand what PVCs are and then discuss everything you need to know about them.
What are PVCs?
PVC is short for Premature Ventricular Contractions. They are also called Ventricular premature beats and Ventricular extrasystoles. In a normal, synchronized heart rhythm, your heart beats in a smooth, steady rhythm thanks to a natural electrical system. It all starts in a small area called the sinoatrial (SA) node, located in the upper right part of your heart. This is your heart’s natural pacemaker — it sends out a signal that tells the top chambers (the atria) to contract and push blood into the lower chambers (the ventricles).
Next, the signal passes through a checkpoint called the atrioventricular (AV) node, which briefly slows things down to give the ventricles time to fill with blood. Then the signal travels down special pathways to the bottom of the heart, making the ventricles contract and pump blood to the lungs and the rest of your body.
But sometimes, things don’t go as planned. In a condition called Premature Ventricular Contractions (PVCs), the signal starts too early, and it comes from the bottom chambers (the ventricles) instead of the top. This early signal can throw off the heart’s normal rhythm, leading to a feeling of a skipped or extra beat. You might feel them as a flutter in the chest, a missed beat, a strong thump, or a momentary pause in your heartbeat
Most PVCs are harmless, especially in individuals with healthy hearts. But in some cases, they may reflect or contribute to heart dysfunction, especially when they occur frequently.
What PVCs Feel Like: Common Symptoms
If you have PVC, you may or may not feel the symptoms. You may discover them only during a routine ECG or check-up. When symptoms do occur, they can include:
- A sensation of skipped or irregular heartbeats
- Chest fluttering
- Chest Thumping,
- Lightheadedness
- Fatigue and mild shortness of breath.
It is necessary to contact your healthcare professional if you have symptoms like fainting.
What Causes PVCs?
PVCs can occur in healthy individuals without any clear reason. However, several triggers and risk factors have been associated with their occurrence.
1. Lifestyle and Non-Cardiac Triggers
Certain daily practices, habits, or conditions that are not directly related to the heart can trigger PVCs. Here are some common triggers:
- Caffeine
- Alcohol
- Tobacco use
- Stress and anxiety
- Sleep deprivation
- Medications (like decongestants or asthma medications)
2. Medical Conditions
Pre-existing medical conditions can trigger PVCs. Here are a few triggers:
- Electrolyte imbalances (low potassium, magnesium, or calcium)
- Anemia
- High blood pressure
- Structural heart disease (like cardiomyopathies or valve disorders)
- Acute events such as heart attacks or myocarditis
PVCs can also occur more frequently with age. Males, African Americans, and individuals with hypertension or bundle branch block are statistically more prone to developing PVCs.
Understanding the risks of PVC
In healthy individuals, occasional PVCs are generally not dangerous. However, their impact depends on several factors, including frequency, symptoms, and underlying heart health.
- Occasional PVCs in healthy individuals are usually benign and don’t require treatment.
- Frequent PVCs (e.g., >10% of total heartbeats in 24 hours) may impair cardiac function.
- Persistent high PVC burden can lead to PVC-induced cardiomyopathy, causing heart muscle weakening and left ventricular dysfunction.
- Nonsustained VT occurs when ≥3 PVCs appear consecutively but resolve within 30 seconds.
- Sustained VT is a serious condition where a rapid heartbeat lasts >30 seconds and may cause syncope or sudden cardiac arrest.
- Symptoms like palpitations, dizziness, or breathlessness alongside PVCs require further clinical evaluation.
- Frequent or symptomatic PVCs should prompt cardiology referral, especially in those with underlying heart disease.
Close Monitoring Needed:
Those with a high PVC burden or preexisting heart conditions need regular follow-ups. Early detection and appropriate management can help reverse damage and significantly improve the quality of life. Continuous ECG monitors can help track PVC burden over time and evaluate treatment effectiveness, especially in individuals at risk of PVC-induced cardiomyopathy.
How Are PVCs Diagnosed?
If you feel unusual heartbeats, your doctor may recommend:
12-lead Electrocardiogram (ECG) – to detect abnormal heartbeats
Holter monitor – a 24 to 48-hour device to track your heart rhythm
Echocardiogram – to check for structural heart problems
Exercise Stress testing – to evaluate how your heart behaves under physical exertion.
Wearable ECG devices – Portable, wearable monitors that continuously track your heart rhythm over days or weeks for irregularities
These tests help rule out underlying heart disease, which is critical in determining if your PVCs are benign or a sign of something more serious.
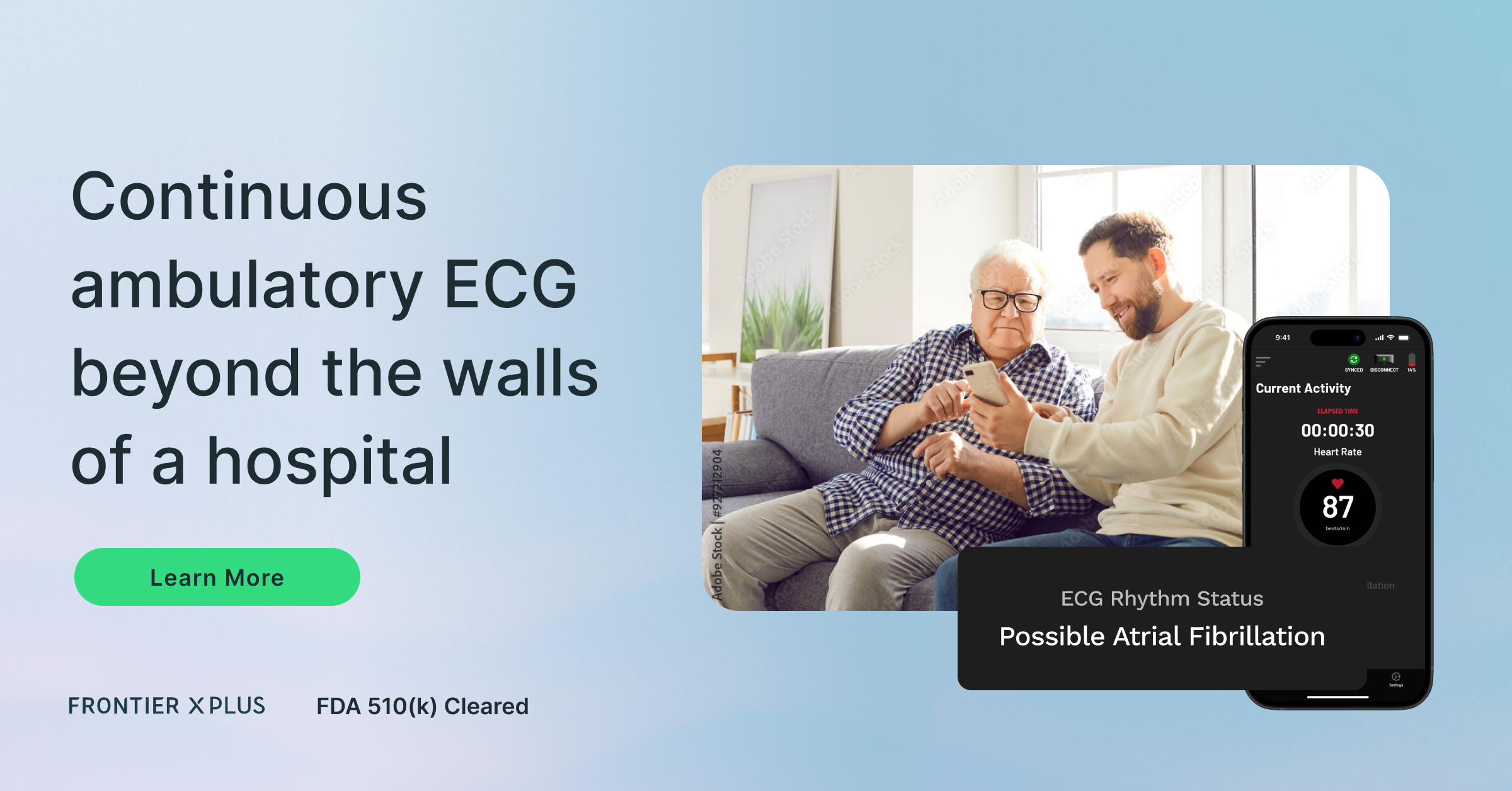
The Role of Wearable ECG Devices
Recent advancements in FDA-cleared wearable continuous ECG monitors have made it easier to detect both symptomatic and silent PVCs. These devices offer continuous, real-time heart monitoring outside of clinical settings, making it possible to track irregular beats over days or weeks and identify high-burden PVCs that may go unnoticed during short ECGs or clinic visits.
Unlike wrist-based devices or traditional Holter monitors that require periodic clinic visits, patchless, chest-worn, medical-grade, continuous ECG monitors like the Frontier X Plus can capture continuous, high-fidelity ECG waveforms in real time for up to 24 hours (or as long as the clinician prescribes), with just an hour of chargingIt enables remote access to ECG data by physicians for early diagnosis, reducing the need for repeated in-clinic testing. Additionally, detailed ECG reports can be downloaded and easily shared with healthcare providers for follow-up, second opinions, or long-term heart health management.
By integrating seamlessly into daily life, the Frontier X Plus offers high-fidelity continuous ECG recording that can aid physicians in early detection of arrhythmias like atrial fibrillation, as well as ongoing evaluation and treatment planning. While the Frontier X Plus does not detect PVCs directly, the ECG data it captures can be reviewed by physicians to assess rhythm patterns. In patients with a known high PVC burden, this data may support long-term monitoring of treatment effectiveness, lifestyle changes, or outcomes post-catheter ablation, with appropriate clinical oversight.
Read More: Continuous ECG Monitoring to Detect Asymptomatic Heart Arrhythmias During Sleep
How Are PVCs Treated?
Treatment is not always necessary for people with no symptoms and low-frequency PVCs.
What can help?
- Lifestyle changes can help manage PVCs:
- Reduce or avoid caffeine and alcohol
- Get adequate sleep
- Manage stress and anxiety
- Avoid stimulants and certain decongestants
2. Medications may be prescribed if symptoms are bothersome:
- Beta-blockers
- Calcium channel blockers
- Antiarrhythmic drugs (in selected cases)
3. If lifestyle changes and medicines don’t have an effect, radiofrequency catheter ablation may be recommended.
Summary
PVCs are common and often harmless, especially in healthy individuals. However, frequent or symptomatic PVCs can indicate underlying cardiac issues and warrant evaluation. With advanced continuous ECG monitoring, you can take charge of your heart health from the comfort of home.
Whether you’re evaluating palpitations or managing a diagnosed arrhythmia, understanding your heart rhythm is the foundation for peace of mind and proactive care.
FAQs
1. Are PVCs life-threatening?
In most healthy individuals, PVCs are harmless. However, in people with heart disease or very frequent PVCs, they can lead to complications if untreated.
2. Do PVCs require lifelong treatment?
Not always. Many people outgrow them, or they reduce with lifestyle changes. Medications or ablation may be needed in persistent or high-burden cases.
3. Is exercise safe with PVCs?
Generally, yes, especially if you don’t have structural heart disease. Still, consult your healthcare professional before starting a workout routine if you have frequent PVCs.
4. Can I monitor PVCs at home?
No. Wearable ECG monitors like the Frontier X Plus allow users to record their heart rhythm continuously. While the device can detect atrial fibrillation, it does not detect PVCs. To identify PVCs or other irregularities, the recorded ECG data must be reviewed by a physician.
5. Can anxiety cause PVCs?
Yes. Stress and anxiety are common triggers. Learning stress-management techniques may help reduce their frequency.
6. When should I see a doctor about PVCs?
If you feel dizzy, faint, have chest pain, or notice frequent irregular heartbeats, you should see a healthcare provider for evaluation.
Related Posts
You might also like
-

Featured Articles
- Why Body Shock Monitoring Is Crucial for Every AthleteJanuary 7, 2026
- Frontier X2 vs Smart Ring: Which Wellness Tracker Knows...November 28, 2025
- The ROI of Investing in Frontier X2 With HSA/FSANovember 21, 2025
- Why Body Shock Monitoring Is Crucial for Every Athlete
CATEGORIES
POPULAR POSTS
- How Cold Weather Can Affect Heart Rhythm Disorders
- Can Overtraining Increase Your Risk of Heart Rhythm Issues
- Frontier X Plus Versus ECG Patches: Which Is Right for Long-Term Heart Rhythm Monitoring?
- Why Sudden Heart Rate Spikes During Exercise Should Not Be Ignored
- Frontier X Plus vs. Handheld Device: Which ECG Monitoring Approach Is Right for You?
-
Follow us on
Top Searches for Heart Health
Top Searches for AFib
Frontier X2 Smart Heart Devices
Top Searches for Heart Rate
VISUAL STORIES