You step outside on a chilly morning and feel that first burst of cold air. It wakes you up instantly. But for people living with congestive heart failure, cold weather can do more than just take your breath away – it can place extra strain on your heart and circulatory system. Let’s unpack exactly how cold weather affects congestive heart failure, the physiological reasons behind it, and how you can protect your heart during the winter months.
This topic is also tied to common search queries such as cold weather and heart health, cold weather heart failure risk, heart rate in cold weather, congestive heart failure winter symptoms, and heart rhythm monitoring in winter.
What Is Congestive Heart Failure?
Congestive heart failure (CHF) is a condition where the heart cannot pump blood as effectively as it should. This does not mean the heart has stopped working. It means the heart struggles to keep up with the body’s demands. Fluid can build up in the lungs, legs, or abdomen, and symptoms like shortness of breath, fatigue, and swelling can occur.
Because CHF affects how your body manages blood flow and pressure, anything that increases stress on your cardiovascular system can worsen symptoms – and cold weather is one of those stressors.
How Cold Weather Stresses the Heart
Cold temperature affects your body in several interconnected ways that can be particularly challenging for someone with congestive heart failure.
1. Cold Causes Blood Vessels To Constrict
When the air is cold, your blood vessels tighten or constrict in order to preserve heat. While this is a normal response, it increases the resistance your heart must work against to pump blood. For someone with heart failure, this added resistance makes it harder for the heart to circulate blood efficiently.
2. Blood Pressure Increases in Cold Weather
Because of vasoconstriction – that narrowing of blood vessels – your blood pressure tends to rise in cold weather. An elevated blood pressure increases the workload on a heart already struggling to pump effectively.
3. Cold Weather Elevates Heart Rate
Your heart beats faster in the cold to maintain body warmth. For someone with congestive heart failure, an increased heart rate can mean that the heart is working harder than it should when it is already compromised.
4. Cold Can Trigger Inflammation and Blood Thickening
Winter air can make blood slightly thicker through dehydration and the body’s protective response. Thicker blood is harder to pump, increasing cardiac workload. Combined with inflammation from respiratory infections like cold and flu that are more common in winter, cold weather creates a perfect storm of cardiovascular stress.
Cold Weather Triggers Common Heart Failure Symptoms
People with congestive heart failure often notice a worsening of symptoms in cold seasons. These may include:
- Shortness of breath with minimal effort
• Increased swelling in legs or feet
• Faster heart rate at rest
• Fatigue and reduced exercise tolerance
• Chest discomfort during exposure to cold
Cold air also causes airways to narrow slightly. This can feel similar to breathlessness from heart failure and makes existing symptoms more noticeable.
Winter Activity and Heart Demand
You might think cold weather simply makes you uncomfortable, but it actually increases your heart’s metabolic demand – even when you are at rest. Your body burns extra energy to maintain core temperature, requiring more blood flow and oxygen. For a heart already compromised by CHF, this extra demand can deplete reserve capacity more quickly.
Even walking on a frosty morning can raise heart rate and blood pressure significantly for people with a compromised heart.
Why Monitoring Matters in Cold Weather
When your heart is under additional stress from environmental factors like cold, chronic conditions like CHF benefit from closer observation. That is where heart rate and rhythm monitoring become valuable tools in your health toolkit.
Devices that offer longer term ECG and heart rate tracking give insight into how your heart responds throughout the day and night – including during cold exposure or winter activity.
How Fourth Frontier Devices Support Heart Monitoring
Modern monitoring tools help you and your clinician understand your heart’s behaviour beyond occasional checks.
The Frontier X Plus is a medical-grade, FDA cleared long term ECG monitor used for clinical rhythm tracking. It records continuous heart rhythm information and allows physicians to observe trends over time. This can be especially useful for people living with heart conditions like congestive heart failure who need precise rhythm data and context around symptoms.
The Frontier X2 is a wellness grade chest worn device that records ECG and heart rate for fitness and wellbeing insight. While it is not a medical device, it provides detailed heart rate data, heart rate variability, and trend information that can support your awareness of how cold weather or exertion affects your heart performance.
Both devices help bridge the gap between occasional heart rate checks and comprehensive trend tracking, empowering you to better understand and manage your heart throughout all seasons.
Winter Health Habits That Help Protect Your Heart
Cold weather is not something you can avoid entirely, but there are practical approaches that help you stay safe and stable throughout winter.
1. Dress Warmly and Protect Your Core
Keeping your body warm reduces the need for vasoconstriction. Wear layers and cover your chest, head, hands and feet when you go outside. A warm core means your heart does not have to work as hard to maintain temperature.
2. Stay Hydrated Even in Cold Weather
You may not feel as thirsty in winter, but dehydration thickens your blood and can raise your heart rate. Drink fluids regularly and include electrolyte balance if needed.
3. Avoid Sudden Exertion in Cold Air
Try to avoid sudden bursts of activity in cold weather such as shovelling snow or sprinting outdoors without a warmup. Your heart responds more dramatically in cold air.
4. Keep Indoor Air Clean and Warm
Dry air in winter can trigger respiratory irritation. Use a humidifier if needed. Improved indoor air quality eases both breathing and heart workload.
5. Maintain Your Heart Medications as Prescribed
Warmer weather changes your medication needs less than cold weather. Winter can change your blood pressure response. Always consult your clinician before making medication adjustments.
The Link Between Respiratory Infections and Heart Strain
Cold weather also increases the prevalence of respiratory infections like flu and bronchitis. These infections not only make breathing difficult but can raise heart rate and inflammatory response.
For people with congestive heart failure, even a mild respiratory infection can increase fluid retention and worsen symptoms. Getting your annual flu shot and staying current with vaccines helps reduce this risk.
When Cold Weather Should Prompt Extra Caution
If you notice the following in cold weather, take it seriously:
- New or worsening shortness of breath
• Increased swelling in legs or abdomen
• Rapid weight gain over days
• Persistent fatigue or inability to exercise
• Heart rate spikes even at low activity
These may indicate that your heart is struggling with the added environmental stress.
Research and Evidence Supporting Cold Impact on Heart Health
Numerous studies show increased cardiovascular risk in colder months. For example, research reports cardiovascular mortality rises in winter, even in regions with milder climates. This is linked to elevated blood pressure, increased sympathetic nervous system activity and higher blood clot risk in the cold.
Understanding these patterns helps you anticipate and manage seasonal heart strain rather than react after symptoms escalate.
How You Can Use Technology to Stay Ahead
Winter is the season when many health insights matter most. Continuous heart rhythm monitoring combined with lifestyle awareness lets you track how your heart reacts in real time and across conditions long term. This data is invaluable in coaching, clinical evaluation, and personalized decision making.
Trends over time – not single readings – help you and your clinician distinguish between normal cold responses and signals of worsening heart function.
Final Thoughts
Cold weather does affect congestive heart failure. It places additional load on your heart through increased blood pressure, faster heart rate, vascular constriction and metabolic demands. When you know how cold impacts your body, you can take proactive steps to protect your heart.
Arming yourself with data, adopting smart winter habits, and partnering with your health care provider will help you stay safer and more comfortable throughout the cold season. Continuous monitoring tools – whether medical grade or wellness grade – can help you see the trends so you are informed rather than surprised.
Your heart never takes a season off. Understanding how weather interacts with your cardiovascular system is part of managing a chronic condition with confidence and control.
FAQs
Can cold weather worsen congestive heart failure
Yes. Cold weather increases blood pressure and heart rate, which places extra strain on the heart and can worsen symptoms of congestive heart failure.
Why does cold temperature affect the heart more than warm air
Cold air causes blood vessels to tighten, which raises blood pressure and makes the heart work harder to circulate blood.
Is it safe to exercise outside with heart failure in winter
You can exercise safely with heart failure in winter if you warm up properly, dress warmly and start with light activity. Always consult your doctor for personalised recommendations.
How does dehydration in cold weather affect heart failure
Dehydration thickens your blood and may increase your heart rate and blood pressure. Staying hydrated helps your cardiovascular system work more efficiently.
Can continuous heart monitoring help manage heart failure in cold weather
Yes. Continuous ECG and heart rate monitoring with tools like Frontier X Plus and Frontier X2 can help track how your heart responds to cold weather and activity, aiding in proactive care.
As an athlete, you push your body to its limits – training hard, competing harder, and always seeking that edge. But in that pursuit, one silent risk often gets ignored: the mechanical impact your body experiences with every stride, jump, or explosive movement. That’s where body shock monitoring comes in – and why it’s becoming a game changer for performance, injury prevention, and long-term resilience.
What Exactly Is Body Shock?
“Body shock” refers to the physical stress and impact forces your body undergoes during high-load activities. Think about a runner’s foot strike, a plyometric jump, or even the repeated dives and landings in basketball. These impacts generate forces that travel through your bones, joints, and soft tissue. Over time, if not monitored, these forces can accumulate and contribute to micro-damage, inflammation, fatigue, or injury.
In sports science, understanding and managing this “mechanical load” – not just how hard your cardiovascular system works – is essential for staying healthy and performing at your best.
Why Monitoring Body Shock Matters for Training and Performance
1. Injury Prevention Through Load Management
Research consistently shows a link between training load and injury risk. A systematic review found moderate evidence that sudden spikes in training load significantly increase the likelihood of injury in athletes.
By monitoring body shock, you’re not just tracking how much work you do, but how much mechanical stress your body actually absorbs. This helps you identify when your load is creeping up dangerously, so you can adjust your training before breakdown happens.
2. Optimizing Recovery and Reducing Overtraining
Your body doesn’t just respond to cardiovascular stress – it also needs time to repair the micro-trauma caused by impact. Excessive body shock without adequate recovery can lead to overtraining or overuse injuries. Overtraining is a state where stress outweighs recovery, causing declining performance, fatigue, or even injury.
When you measure body shock, you gain a powerful internal feedback tool. You can decide when to dial back, rest, or cross-train – rather than blindly pushing harder.
3. Fine-Tuning Technique and Equipment
Impact isn’t only about volume – it’s also about form, surface, and equipment. Monitoring body shock allows you to evaluate how changes in technique, footwear, or running surface affect the force your body experiences.
For example, if you switch to a more cushioned shoe but see a rise in shock readings, it might suggest that your form or biomechanics need to adjust. This insight helps you optimize both your training and your gear.
4. Balancing Load and Longevity
Athletes who consistently track internal and external load often find a “sweet spot” – a level where performance improves without pushing their injury risk too high. Monitoring body shock adds another layer to that by focusing on biomechanical load. For long-term health, being mindful of these forces can mean fewer stress-related injuries, better joint health, and a longer, more sustainable athletic career.
How Body Shock Monitoring Fits into Modern Athlete Monitoring
Body shock monitoring is part of a broader philosophy in modern training: internal vs external load. External load refers to what you do (distance, reps, time), and internal load refers to how your body responds (heart rate, perceived exertion, recovery markers).
Monitoring only one dimension can leave you blind to risk. High-volume training might feel fine cardio-wise, but if your shock load is too high, your tissues may be paying the price in silent stress.
Tools that measure body shock help you connect these two dimensions, giving you a richer, more complete picture of training stress.
How Sensors Make This Possible
Wearable sensor technology has matured dramatically. Modern wearables often combine accelerometers (to detect movement and impact) with physiological sensors (like ECG or heart rate) to deliver a multidimensional understanding of load.
Using these sensors, you can track not just how stressed your heart is, but how jarring each training session is for your joints, muscles, and connective tissue.
The Role of Continuous ECG and Devices Like Frontier X2
To get a full picture of your body’s response to training, combining body shock data with cardiovascular insights is powerful. Devices like the Frontier X2 capture not only heart rate variability, breathing rate, and ECG data, but also body shock. This gives you a holistic view: when impact is high, how is your heart coping? Are you recovering well?
For athletes needing deeper clinical-level data, medical-grade ECG monitors like Frontier X Plus (which allow extended ECG tracking) bridge the gap between wellness tracking and medical monitoring. This helps you and your coach or medical team spot unusual heart responses, overtraining signs, or recovery issues – all while keeping an eye on your mechanical stress.
Real-World Examples: Where Body Shock Monitoring Helps
- Runners: You may realize that changing from hard pavement to a softer trail actually reduces body shock, helping reduce knee or shin stress.
- Jump athletes / basketball players: Tracking shock during plyometric workouts can help you monitor how your body handles repetitive impact and whether you need more recovery.
- Strength athletes: Even in lifting, body shock (or its analogs) can help assess how much stress your musculoskeletal system takes from heavy lifts, enabling smarter progression.
- Team sports: Using shock monitoring during training and matches helps identify load patterns that predict injury risk, particularly in high-impact drills.
Benefits You Actually Feel (and Avoid)
By monitoring body shock, you’re investing in:
- Smarter training: You train hard but not recklessly.
- Better recovery: You can see clearly when your body needs rest.
- Injury reduction: You catch risky patterns before they become real injuries.
- Improved longevity: Your joints, tendons, and muscles stay healthier.
- Data-driven decisions: Technique tweaks, gear changes, and recovery tweaks become more precise and informed.
Final Thoughts
If you take one thing away, let it be this: your training risk isn’t just determined by how hard you push your heart – but also by how hard you hit the ground. Monitoring body shock elevates your awareness from “how tired am I” to “how worn am I,” giving you the insight you need to train smarter, recover better, and stay injury-free.
In today’s era of data-driven athletic performance, body shock monitoring isn’t a luxury – it’s an essential part of the toolkit for any serious athlete. Use it wisely, and you’ll not just be stronger, but smarter.
FAQs
Q1: What is body shock in sports training?
Body shock refers to the mechanical impact forces your body receives during athletic movements, like running, jumping, or landing. Monitoring body shock helps assess how much stress your musculoskeletal system experiences and can guide training to reduce injury risk.
Q2: How does body shock monitoring help prevent injury?
By tracking impact forces over time, you can identify dangerous load patterns (like sudden spikes or repetitive high-impact sessions) and adjust your training before injury occurs.
Q3: Can body shock data improve my recovery?
Yes – paired with physiological metrics like heart rate variability and ECG data, body shock helps you understand both how hard you hit and how well your body recovers, so you know when to rest or push.
Q4: What devices can I use to monitor body shock?
Wearable monitors like the Fourth Frontier X2 provide real-time body shock tracking along with ECG, HRV, and breathing metrics. For deeper clinical insight, a medical-grade ECG device like Frontier X Plus can be used.
Q5: Is body shock monitoring only for elite athletes?
Not at all. While it’s especially useful for high-performance athletes, any athlete – whether recreational or competitive – can benefit from understanding and managing biomechanical load to reduce injury and optimize training.
You lace up your running shoes with one goal in mind. To run better. Maybe that means going faster. Maybe it means running farther. Or maybe it simply means feeling stronger without burning out. No matter your goal, there is one invisible factor that decides how well you train and how well you recover. Your heart rate zone.
Most runners train based on pace, distance, or how tired they feel. But elite runners know something most amateurs overlook. Real progress happens when you train in the right heart rate zone for your body. Not too easy. Not too hard. Just precise enough to stimulate adaptation without overstressing your system.
When you learn to run in the right zone, you stop guessing. You start training smarter.
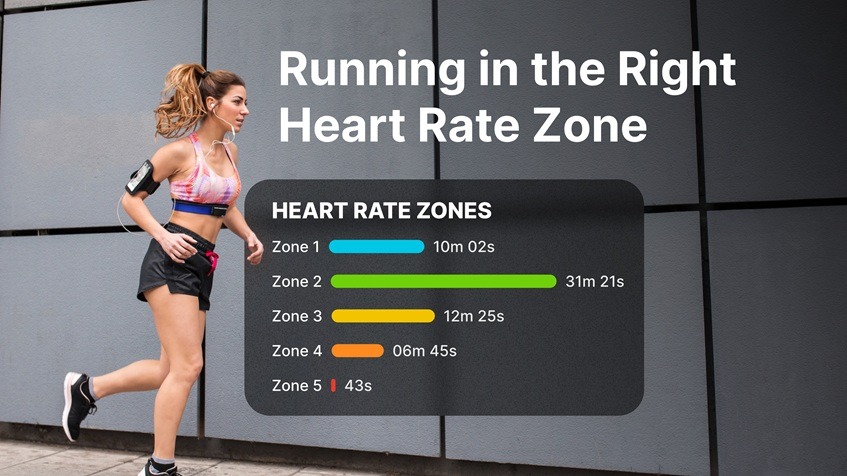
What Heart Rate Zones Really Mean for Runners
Your heart rate zone describes how hard your cardiovascular system is working during a run. Each zone trains a different energy system and produces a different adaptation.
Here is what most runners work with:
- Zone 1 very light effort for recovery runs
- Zone 2 aerobic base building and fat utilization
- Zone 3 moderate intensity endurance development
- Zone 4 high intensity effort improving speed and stamina
- Zone 5 maximum effort sprint capacity
If you always run hard, your body never fully recovers. If you always run easy, your performance plateaus.
Real progress happens when you cycle between these zones intentionally.
Why Most Runners Train in the Wrong Zone
Here is the truth most runners do not want to hear.
Most people think they are training hard when they are actually training in a gray zone. Too hard to build proper endurance. Too easy to develop speed. That zone leads to fatigue without meaningful fitness gains.
Common mistakes include:
- Running every session at the same moderate effort
- Ignoring recovery zones
- Chasing pace instead of physiological response
- Training based on emotion instead of data
When you train like this, your heart is working harder than you realize. And your recovery suffers quietly in the background.
What Happens When You Run in the Right Heart Rate Zone
When your training is guided by heart rate zones, your results become predictable.
You begin to notice:
- Faster recovery between runs
- Improved aerobic capacity
- Better running economy
- Reduced risk of overtraining
- More consistency week after week
Your heart adapts gradually. It pumps blood more efficiently. Oxygen delivery improves. Fat utilization becomes stronger. And your endurance increases without burning you out.
You stop feeling stuck. You start feeling in control.
How the FX2 Supports Smarter Zone Based Training
The Frontier X2 is a wellness grade device designed to record heart rate and ECG data for fitness and training insights. When you run with FX2, you gain visibility into how your heart responds to each session instead of relying only on effort or pace.
This allows you to:
- Observe how long you stay in each heart rate zone
- Track how fast your heart recovers after intervals
- Understand how your body responds to hill runs or long runs
- See how stress sleep and hydration affect your running performance
You are no longer guessing whether a run was easy or hard on your system. You can see it.
Why Heart Rate Based Training Improves Endurance Faster
Your pace can drop on a bad sleep day. Your energy can fluctuate with nutrition. But your heart never lies about internal effort.
Heart rate based training helps you:
- Keep easy runs truly easy
- Push hard only when your body is ready
- Prevent unnecessary fatigue accumulation
- Maximize the benefit of every session
This is why many endurance coaches now prioritize heart based training over pace only programs.
The Role of Medical Grade and Wellness Monitoring in Running
Medical grade tools like the Frontier X Plus provide long term ECG monitoring support in clinical settings and are FDA cleared for heart rate and rhythm trend assessment under physician supervision.
Wellness grade tools like the Frontier X2 allow runners to record ECG and heart rate data for fitness tracking and training insights. These tools do not replace medical diagnosis. They support long term awareness of how your heart responds to training load recovery and daily stress.
For runners who train consistently, this ability to observe long term trends can add an important layer of safety and intelligence to training decisions.
How Training in the Wrong Zone Slows Your Progress
When you train too hard too often:
- Resting heart rate stays elevated
- Recovery between sessions worsens
- Sleep quality declines
- Motivation drops
- Injury risk rises
When you train too easy all the time:
- Speed plateaus
- Stamina stagnates
- Race performance suffers
The right zone balance keeps you progressing without breaking down.
How to Set Your Heart Rate Zones for Running
Most runners use one of the following methods:
- Percentage of maximum heart rate
- Heart rate reserve method
- Lactate threshold based zones
While formulas give estimates, your real zones evolve with training. This is why long term tracking matters. Your true aerobic zone today may shift as your conditioning improves.
What Smarter Run Training Looks Like in Practice
A balanced week often includes:
- One long aerobic zone run
- One speed or interval session
- One tempo or moderate endurance run
- One light recovery run
Each session serves a purpose. Each zone is trained intentionally. And your heart guides the intensity instead of ego.
How Heart Rate Data Protects You From Overtraining
Early signs of overload often show up in heart response before your muscles feel it.
Watch for:
- Elevated resting heart rate
- Slower recovery after intervals
- Higher heart rate at the same pace
- Persistent fatigue across sessions
These signals tell you when it is time to adjust load instead of pushing harder.
Why Running Smarter Beats Running Harder
Elite runners do not train hard every day. They train precisely.
They protect their aerobic base. They apply intensity only when planned. And they prioritize recovery as much as effort.
When you adopt this mindset, your training becomes sustainable. You do not burn out mid season. Your performance peaks when it matters.
The Long Term Benefits of Zone Based Training
When you commit to smarter heart guided running, you gain:
- Stronger aerobic foundation
- Better fat utilization
- Faster post run recovery
- Improved race pacing
- Greater mental confidence during long runs
You stop fearing fatigue. You start managing it.
Final Takeaway
Your pace measures how fast you move. Your heart rate reveals how hard your body is working.
When you train in the right heart rate zone, every run becomes purposeful. Every session adds value. Every recovery day actually restores you.
Tools like the Frontier X2 give you visibility into how your heart behaves during training. The Frontier X Plus supports medical supervision when deeper cardiovascular insight is required. Together, they help bridge the gap between effort and intelligent endurance training.
If you want to run longer, faster, stronger, and safer – you need to run in the right zone.
FAQs
- What is the best heart rate zone for endurance running
Most endurance development happens in zone two where your aerobic system improves and fat utilization increases. - Is heart rate training better than pace based training
Heart rate reflects internal effort while pace reflects external speed. Using both together produces the best results. - Can heart rate monitoring prevent overtraining in runners
Long term heart rate trend tracking helps detect early fatigue and recovery imbalance before performance declines. - How does ECG monitoring help runners
ECG monitoring supports awareness of heart rhythm and rate trends over time allowing athletes and physicians to observe how training stress influences the heart. - Is FX2 suitable for long distance running
Yes the Frontier X2 is designed for wellness grade heart rate and ECG data tracking during extended training sessions.
When you think of a heart attack, you probably imagine someone clutching their chest in sudden, sharp pain. But what if a heart attack could happen quietly, without any warning signs or pain? This is known as a silent heart attack, and it’s far more common than most people realize. In fact, many people only discover they’ve had one after undergoing an ECG or imaging test for another reason.
In this blog, we’ll break down what a silent heart attack is, how it differs from a typical one, why it happens, and how you can protect yourself using modern heart monitoring technologies.
What Is a Silent Heart Attack?
A silent heart attack, or silent myocardial infarction (SMI), occurs when blood flow to part of the heart muscle is blocked – just like in a traditional heart attack – but without the intense chest pain or obvious symptoms.
The heart muscle still suffers damage from the lack of oxygen, but because you might not feel typical warning signs, you could miss it entirely.
Studies suggest that 1 in every 5 heart attacks is silent. This means thousands of people go about their daily lives unaware that their heart has been injured.
Why Do Silent Heart Attacks Happen?
Several factors can make a heart attack “silent.” Some people may have a higher pain threshold, while others – such as those with diabetes – may have nerve damage (neuropathy) that dulls pain perception.
Common causes and risk factors include:
- High blood pressure and high cholesterol
- Diabetes (which affects nerve sensitivity)
- Smoking and alcohol consumption
- Obesity and sedentary lifestyle
- Family history of heart disease
- High stress levels
- Poor diet high in saturated fats or processed foods
Even without noticeable pain, your heart still suffers damage during these episodes – making it crucial to detect them early.
Subtle Signs You Might Have Had a Silent Heart Attack
You might not feel crushing chest pain, but your body often gives more subtle clues.
Look out for:
- Unexplained fatigue or weakness, even after rest
- Mild discomfort in the chest, upper back, neck, or jaw
- Shortness of breath, especially with light exertion
- Cold sweats or sudden lightheadedness
- Indigestion-like discomfort or nausea
These symptoms may come and go or feel so mild that you dismiss them as stress, heartburn, or fatigue. But if they recur or persist, it’s important to talk to your doctor.
Why Silent Heart Attacks Are Dangerous
The biggest danger of a silent heart attack is delayed diagnosis. Because it goes unnoticed, you might not receive timely treatment – which means heart muscle damage continues to accumulate.
This can increase your risk of:
- Heart failure
- Arrhythmias (abnormal heart rhythms)
- Another, more severe heart attack
- Sudden cardiac arrest
Silent heart attacks often indicate underlying coronary artery disease (CAD) – the buildup of plaque in your arteries. Early detection and continuous monitoring can dramatically reduce future risk.
How Doctors Detect a Silent Heart Attack
Even if you’ve had no symptoms, certain medical tests can reveal signs of past or ongoing heart damage.
Common diagnostic tools include:
- Electrocardiogram (ECG or EKG): Detects abnormal electrical patterns caused by past heart muscle injury.
- Echocardiogram: Uses ultrasound to visualize heart muscle movement and detect areas of reduced function.
- Blood tests: Measure cardiac enzymes like troponin that rise after heart muscle injury.
- Cardiac MRI or CT scan: Provides detailed imaging of heart tissue and blood vessels.
Preventing Silent Heart Attacks: Steps You Can Take
The good news is that heart attacks – silent or otherwise – are largely preventable. Small, consistent lifestyle changes can make a big difference.
- Get your numbers checked: Regularly monitor your blood pressure, cholesterol, and blood sugar.
- Eat heart-healthy foods: Choose more fruits, vegetables, whole grains, lean proteins, and healthy fats.
- Exercise regularly: Even 30 minutes of brisk walking most days can improve heart function and circulation.
- Manage stress: Chronic stress contributes to inflammation and hypertension. Practices like meditation, yoga, or deep breathing can help.
- Avoid smoking: Tobacco directly damages your arteries and accelerates plaque buildup.
- Schedule regular heart check-ups: Especially if you have a family history of heart disease.
The Role of ECG Monitoring in Detecting Silent Heart Problems
Modern ECG-based monitoring tools make it easier than ever to capture detailed cardiac data that traditional check-ups might miss.
The medical-grade Frontier X Plus is an FDA-cleared, prescription-based long-term ECG monitor designed to record heart rhythm data over extended periods. It provides high-fidelity ECG insights that help physicians interpret rhythm trends and assess cardiac performance over time in individuals being evaluated for conditions such as atrial fibrillation, tachycardia, or bradycardia.
Meanwhile, the Frontier X2 serves as a wellness-grade device for continuous ECG and heart rate recording during workouts or daily life. It helps you track cardiac effort, recovery, and performance trends, offering valuable feedback on how your heart responds to different levels of activity and stress.
Together, these tools provide you and your physician with meaningful data to better understand your heart’s behavior – even when you may not feel any symptoms.
FAQs
- Can a heart attack happen without chest pain?
Yes. Silent heart attacks occur without the typical chest pain. You might only feel fatigue, breathlessness, or mild discomfort, but the heart still suffers damage. - How do doctors detect a silent heart attack?
An ECG or echocardiogram can reveal abnormal patterns or tissue damage from a past attack. Blood tests for cardiac enzymes may also help identify recent silent events. - Who is most at risk of a silent heart attack?
People with diabetes, older adults, and those with high blood pressure or cholesterol are more likely to have a heart attack without obvious pain. - Can a silent heart attack lead to heart failure?
Yes. Repeated silent heart attacks can weaken the heart muscle, eventually leading to heart failure or arrhythmias. - How can I monitor my heart health at home?
You can use devices like the Frontier X Plus (a medical-grade, FDA-cleared long-term ECG monitor) or the Frontier X2 (a wellness-grade ECG tracker) to record your heart’s electrical activity during daily life. These devices capture ECG data and trends, enabling physicians to review and interpret the information to support timely medical assessment and guide overall heart health management.
Takeaway
A silent heart attack doesn’t scream for attention – but it leaves a lasting mark on your heart. Listening to your body, getting regular check-ups, and using advanced heart monitoring tools can help you detect issues early and protect your heart health for the long term.
If you’ve ever felt unexplained fatigue, breathlessness, or mild chest pressure, don’t brush it off. Your heart might be trying to tell you something – quietly, but urgently.
If your cardiologist has recommended a stress test, you might wonder whether you’ll be asked to walk on a treadmill or simply lie down while receiving medication that “stresses” your heart. Both tests aim to evaluate how your heart performs under strain – but the method, experience, and insights they provide differ significantly. Let’s explore what each type of stress test means, how they work, and which one might be more suitable for you.
What Is a Stress Test and Why Is It Done?
A cardiac stress test measures how your heart responds to exertion. During physical activity, your heart must pump harder and faster to supply oxygen-rich blood to your body. For some people, this added workload may reveal hidden signs of coronary artery disease (CAD), irregular heart rhythms, or inadequate blood flow that might not appear at rest.
Cardiologists typically recommend a stress test when you experience symptoms such as:
- Chest pain or discomfort during exertion
- Shortness of breath
- Unexplained fatigue
- Dizziness or irregular heartbeat
Treadmill Stress Test: The Traditional Approach
The treadmill (exercise) stress test is the most common type of cardiac stress test. It involves walking on a treadmill (or sometimes pedaling a stationary bike) while connected to an ECG machine. The treadmill gradually increases in speed and incline every few minutes to simulate increasing levels of exertion.
What It Measures:
- Heart rate and rhythm (via ECG leads on your chest)
- Blood pressure changes during activity
- Symptoms such as chest pain, fatigue, or breathlessness
- Oxygen consumption and recovery rate
What the Results Show:
This test helps doctors identify whether your heart is getting enough blood and oxygen during exercise. A normal result means your heart handles physical stress well, while abnormal results may indicate possible blockages in coronary arteries, poor exercise tolerance, or arrhythmias triggered by exertion.
Pharmacologic Stress Test: An Alternative for Non-Exercisers
A pharmacologic (chemical) stress test is designed for people who cannot safely perform physical exercise due to age, joint problems, or other health limitations. Instead of walking on a treadmill, medication is administered to make your heart react as if you were exercising.
Common drugs used include adenosine, regadenoson (Lexiscan), dobutamine, or dipyridamole. These medications increase blood flow or heart rate, simulating the effects of physical exertion.
What It Measures:
- ECG changes caused by the induced stress
- Blood pressure and heart rate response to the medication
- Blood flow patterns on imaging scans (if combined with nuclear or echocardiographic testing)
What the Results Show:
Just like the treadmill test, the pharmacologic version helps identify restricted blood flow, abnormal heart rhythms, and areas of the heart not receiving enough oxygen.
Treadmill vs Pharmacologic: Key Differences
| Feature | Treadmill Stress Test | Pharmacologic Stress Test |
| How it works | Physical exercise increases heart workload | Medication mimics exercise effects |
| Ideal for | Patients who can walk/run | Patients unable to exercise |
| Heart rate control | Natural increase with exertion | Drug-induced response |
| Imaging | Often ECG only | Often combined with imaging (echo or nuclear) |
| Duration | 10–15 minutes | 30–60 minutes |
| Preparation | Wear running shoes, avoid caffeine | Avoid caffeine and certain medications |
| Sensation | Physical fatigue or breathlessness | Warm sensation or chest tightness due to medication |
Which Test Is Right for You?
The decision depends on your physical ability, age, and overall cardiovascular risk. If you can walk comfortably, the treadmill test provides a more natural reflection of real-world exertion. However, if arthritis, balance issues, or other conditions prevent safe exercise, your doctor may recommend a pharmacologic stress test instead.
In some cases, a combination test (exercise stress test with echocardiography or nuclear imaging) may be used to obtain a clearer picture of how your heart muscle and blood flow respond to stress.
Understanding Your Results
Your cardiologist will interpret your stress test based on ECG readings, blood pressure response, and any reported symptoms. Possible outcomes include:
- Normal response: Your heart functions well under stress.
- Abnormal ECG patterns: Possible reduced blood flow or rhythm disturbances.
- Blood pressure changes: May indicate vascular or cardiac inefficiency.
- Exercise limitation: Could suggest cardiac or respiratory constraints.
Remember, an abnormal result doesn’t always mean a serious problem – it simply means further testing or evaluation may be required.
The Role of Continuous Heart Monitoring Between Tests
While stress tests provide a controlled snapshot of how your heart performs under exertion, your heart’s rhythm and function can vary widely during everyday activities – from climbing stairs and commuting to moments of rest and sleep.
That’s where long-term heart monitoring becomes invaluable.
The Frontier X Plus is a medical-grade, FDA-cleared, prescription-based ECG monitor designed for extended recording of heart activity in real-world conditions. The data it captures can enable physicians to review rhythm patterns and assess overall cardiac performance over time, beyond what short-term clinical tests can show.
The Frontier X2, in contrast, is a wellness-grade ECG and heart rate monitor that helps users track exertion, recovery, and breathing patterns during workouts or daily routines.
Together, these devices provide complementary perspectives – one supporting physician-guided cardiac review and the other empowering personal health awareness – helping users and their care teams make more informed decisions about long-term heart health and fitness.
Lifestyle Tips to Support Heart Performance
Whether you’re preparing for a stress test or monitoring your heart at home, these tips can help you maintain cardiovascular strength and endurance:
- Exercise regularly: Aim for 150 minutes of moderate activity each week.
- Maintain a balanced diet: Focus on fiber, lean protein, and omega-3 fats.
- Avoid smoking and excess alcohol.
- Monitor blood pressure and cholesterol.
- Manage stress: Breathing exercises and mindfulness can regulate your heart rate.
- Get enough sleep: Poor sleep can raise heart rate variability and stress load.
FAQs on Stress Tests
- Is a treadmill stress test painful?
No. It involves gradual exertion under supervision, and you can stop anytime you feel uncomfortable. - How do I prepare for a stress test?
Avoid caffeine, alcohol, and heavy meals before the test. Wear comfortable clothing and follow your doctor’s medication instructions. - Which test is more accurate – treadmill or pharmacologic?
Both are reliable when done correctly. The choice depends on your ability to exercise and your cardiologist’s recommendation. - How long does it take to get results?
Initial ECG results are often available right after the test, but if imaging is involved, detailed reports may take a few days. - Can I monitor my heart trends at home?
Yes. You can track your heart’s activity at home using wellness tools like the Frontier X2, which records ECG and heart rate during daily routines or workouts – helping you observe personal trends in exertion and recovery.
For clinical oversight, the Frontier X Plus offers medical-grade, FDA-cleared, long-term ECG recording, enabling physicians to review and assess your cardiac rhythm patterns more comprehensively over time.
Final Takeaway
Both treadmill and pharmacologic stress tests are essential tools for evaluating heart function – one tests your physical endurance, the other your heart’s reaction to medication-induced stress. Whichever method your doctor chooses, it provides valuable insight into how well your heart handles strain.
And for those who wish to stay proactive between checkups, continuous ECG and heart rate tracking using tools like the Frontier X2 can help you better understand your wellness trends, fitness load, and recovery – empowering you to maintain a stronger, healthier heart.
Heart disease is the leading cause of mortality worldwide, and two terms you’ll often hear in this context are Coronary Artery Disease (CAD) and Ischemic Heart Disease (IHD). Many people – even patients and sometimes clinicians – use them interchangeably, but they are not exactly the same. Understanding the distinction can help you recognize symptoms early, seek timely medical care, and explore modern tools like ECG monitoring to protect your heart health.
What Is Coronary Artery Disease (CAD)?
Coronary Artery Disease refers specifically to a condition where the coronary arteries, the vessels that supply oxygen-rich blood to the heart, become narrowed or blocked. This narrowing usually happens due to atherosclerosis – the buildup of fatty deposits, cholesterol, and calcium (known as plaque) inside the arteries.
When the arteries are narrowed, blood flow to the heart muscle is reduced, increasing the risk of chest pain (angina), shortness of breath, or even myocardial infarction (heart attack).
Common CAD symptoms include:
- Pressure or pain in the chest (angina)
- Shortness of breath during exertion
- Fatigue or weakness
- Pain radiating to the neck, jaw, shoulders, or arms
CAD is often described as the most common type of heart disease and is sometimes referred to as arteriosclerotic cardiovascular disease or atherosclerotic heart disease in medical literature.
What Is Ischemic Heart Disease (IHD)?
Ischemic Heart Disease is a broader term that refers to any heart problem caused by reduced blood supply (ischemia) to the heart muscle. While CAD is the leading cause of ischemia, other factors – such as severe anemia, coronary artery spasms, or microvascular dysfunction – can also trigger it.
In other words, all CAD is ischemic heart disease, but not all ischemic heart disease is CAD.
For example:
- CAD-related ischemia: Blocked arteries leading to chest pain.
- Non-CAD ischemia: Severe anemia or coronary spasms reducing oxygen supply even if arteries are not significantly narrowed.
IHD symptoms can include:
- Chest pain (angina)
- Palpitations or irregular heartbeats (atrial arrhythmia)
- Dizziness or fainting
- Heart failure symptoms like swelling in the legs and fatigue
Key Differences Between CAD and IHD
| Aspect | Coronary Artery Disease (CAD) | Ischemic Heart Disease (IHD) |
| Definition | Narrowing/blockage of coronary arteries due to plaque buildup | Any condition where blood supply to heart muscle is insufficient |
| Cause | Mainly atherosclerosis (plaque buildup) | CAD + other causes (anemia, coronary spasms, microvascular issues) |
| Scope | More specific term | Broader umbrella term |
| Symptoms | Angina, chest tightness, heart attack risk | Angina, arrhythmias, heart failure, ischemic cardiomyopathy |
| Diagnosis | Coronary angiography, CT scans, stress tests | ECG, continuous ECG, echocardiography, perfusion scans, angiography |
| Treatment | Medications, stents, bypass surgery | Treating underlying cause (CAD + non-CAD ischemia management) |
Why Early Detection Matters
Both CAD and IHD can progress silently for years before showing obvious symptoms. Sometimes, the first sign of CAD or IHD may be a heart attack. That’s why early detection through regular check-ups and screening is crucial.
Warning signs that may suggest heart ischemia include:
- Chest discomfort even at rest
- Shortness of breath while lying down
- Unexplained fatigue
- Sudden dizziness or fainting spells
- Palpitations
If you notice these signs of clogged arteries in the heart or plaque in arteries symptoms, consult your doctor immediately.
Diagnosis of CAD and IHD
Doctors rely on a combination of tests to diagnose CAD disease and ischemic heart conditions:
- Electrocardiogram (ECG or EKG): Detects ischemia, arrhythmias, or prior heart attacks.
- ECG Monitoring: Chest-strap wearable ECG monitors, such as the Frontier X Plus, enable long-term recording of heart rhythm during daily activities, exercise, and sleep. This allows physicians to review rhythm trends and assess cardiac responses over time as part of a comprehensive clinical evaluation.
- Stress Tests: Measure heart function during exertion.
- Coronary CT Angiography (CCTA): Provides imaging of plaque and narrowing.
- Cardiac Catheterization (Angiogram): The gold standard for identifying arterial blockages.
- Echocardiogram: Ultrasound imaging to assess heart function.
Treatment for CAD and IHD
1. Lifestyle Modifications
- Quit smoking
- Eat a heart-healthy diet low in saturated fats and sugars
- Exercise regularly but safely (under medical supervision if diagnosed with heart disease)
- Manage stress and sleep conditions
2. Medications
- Antiplatelets (e.g., aspirin): To prevent blood clots
- Statins: To lower cholesterol
- Beta-blockers and calcium channel blockers: To control blood pressure and reduce strain on the heart
- Nitrates: To relieve angina symptoms
These are often referred to as CAD disease treatment drugs or ischemic heart disease management therapies.
(Important: The medications listed below are for general awareness only. Treatment should always be determined by a qualified physician. Never start, stop, or adjust any medication without consulting your healthcare provider.)
3. Interventional and Surgical Treatments
- Angioplasty with Stent Placement: Opens blocked arteries
- Coronary Artery Bypass Grafting (CABG): Reroutes blood flow around blocked arteries
- Advanced therapies for ischemic heart failure if the heart muscle has been significantly weakened
The Role of Long-Term ECG Monitoring
Modern longterm ECG monitors like the Frontier X Plus play a critical role in early detection and management of arrhythmias. Chest-strap wearable ECG monitors, such as the Frontier X Plus, enable long-term recording of heart rhythm during daily activities, exercise, and sleep. This allows physicians to review rhythm trends and assess cardiac responses over time as part of a comprehensive clinical evaluation.
For patients with suspected cardiac ischemia or ischemic arrhythmias, continuous monitoring can:
- Detect silent ischemic episodes that occur without chest pain
- Capture arrhythmias related to ischemic heart disease
- Provide data to physicians to personalize treatment
- Help patients track changes during exercise or stress
By spotting problems earlier, continuous ECG monitoring empowers patients and doctors to reduce the risk of heart attack, ischemic heart failure, or sudden cardiac arrest.
Conclusion
While Coronary Artery Disease (CAD) and Ischemic Heart Disease (IHD) are closely linked, they are not identical. CAD is a major cause of IHD, but ischemia can also result from other conditions. Understanding this distinction helps in recognizing symptoms, seeking appropriate treatment, and adopting preventive strategies.
With lifestyle changes, medical therapy, and advanced tools like continuous ECG monitoring, patients can detect problems early and significantly reduce their risk of heart disease.
FAQs
- Are coronary artery disease and ischemic heart disease the same?
Not exactly. CAD is a type of ischemic heart disease caused by blocked coronary arteries, but ischemia can occur from other factors too. - What are the early signs of clogged arteries in the heart?
Chest discomfort, shortness of breath, unusual fatigue, or pain in the arm, neck, or jaw can indicate artery narrowing. - How is CAD diagnosed?
Diagnostic tests may include ECG, continuous ECG monitoring, coronary angiography, echocardiography, and stress tests. - What is the best treatment for CAD?
Treatment for CAD includes lifestyle changes, medications like statins or beta-blockers, and in severe cases, angioplasty or bypass surgery. - Can ECG monitoring support evaluation of ischemic heart disease?
Yes. Long-term ECG recordings can capture heart-rhythm and rate patterns during daily activities that may not appear during clinic tests, enabling physicians to review trends and correlate them with symptoms as part of a broader clinical evaluation. - Does ischemic heart disease always lead to heart failure?
Not always, but untreated or severe ischemia can weaken the heart muscle over time, leading to ischemic heart failure.
Long distance cycling pushes your body in ways that only a handful of other endurance sports do. The climbs, the heat, the hours of steady effort, the sudden bursts of power, the stress of descents, the recovery periods between intervals, all these influence how your heart behaves. If you have ever finished a ride wondering why your heart rate suddenly spiked on a mild climb or why your legs felt strong but your breathing did not match the effort, you are not alone. Cyclists across the world are beginning to realise something important. The key to better performance and better health is hidden right inside your own heart data.
And that is exactly where continuous ECG data becomes a powerful tool. When you see how your heart responds to real world effort in real time, the way you ride, train and recover begins to change.
Today, continuous ECG is no longer something limited to hospitals and clinical labs. Cyclists can now observe detailed heart signals during long rides, helping them understand strain, recovery and early warning patterns that simple Heart Rate numbers cannot show. We take you through what continuous ECG during long rides means, what you can learn from Frontier X2-style ECG data and how long term monitoring with wellness and medical devices fits into your training and overall safety.
Why Cyclists Need More Than Just Heart Rate
Most cyclists train with heart rate monitors or smartwatches. They are great tools, but there is one big limitation. They only show how fast your heart is beating, not how well it is beating.
Two riders can show the same heart rate of 165 beats per minute. One might be perfectly stable and efficient while the other could be showing irregular variations, inefficient electrical activity or early signs of heart stress. Heart rate does not tell you that story.
Continuous ECG, on the other hand, shows the electrical behaviour of your heart throughout your ride. It gives you a moment by moment picture of how your heart handles load, fatigue, heat, dehydration, elevation and stress.
What Continuous ECG Reveals During Long Rides
1. Effort zones that actually match your physiology
You may think you are in Zone 2, but your heart may be showing electrical stress patterns that suggest you are pushing harder than you realise. Continuous ECG helps you learn the truth about your zones. Over time, you can match your perceived effort to your actual cardiac response, improving both safety and performance.
2. Early signs of overheating and dehydration
Long rides in heat can silently strain your heart. ECG patterns often show subtle shifts even before your heart rate rises dramatically. These changes can help you correct your hydration or cooling strategies early.
3. How your heart behaves during climbs versus flats
Climbing is where your cardiac workload spikes. ECG data can show how stable your heart is during long climbs, how quickly it adapts to gradient changes and how effectively it recovers on descents. For cyclists who frequently ride hilly routes, this insight is invaluable.
4. Stress reactions during sudden accelerations
Surges, sprints and gear changes create rapid changes in cardiac load. ECG signals show how abrupt these transitions are for your heart. If the patterns repeatedly show instability, you know exactly which parts of your ride need better conditioning.
5. How fatigue affects your electrical stability
Toward the end of a ride, fatigue shows up in your heart far before your legs feel heavy. Continuous ECG can reveal increased variability, erratic contractions or stress signatures. Knowing this helps you plan rest intervals and nutrition.
The Frontier X2 Advantage: What Cyclists Learn From This Style of Data
Cyclists who use ECG recording devices during training often report specific discoveries that changed the way they ride:
You learn the difference between fitness fatigue and cardiac strain: Two riders can feel equally tired, but their ECG traces tell completely different stories. This helps you avoid pushing through the wrong kind of fatigue.
You discover how poorly timed nutrition affects your heart: Bonking, sudden drops in glucose and electrolyte imbalance all leave cardiac signatures. Over time, you begin to fuel with better timing.
You understand your recovery window better: Your post-ride-ECG patterns can show how quickly your heart settles back into a stable rhythm. This helps you plan training blocks more effectively.
You can identify patterns across weeks of training: Long term trends help you see whether your heart is adapting well or if there are periods where stress load is rising too quickly.
How Frontier X Plus and Frontier X2 Fit Into Long Ride Monitoring
If you are exploring long term heart monitoring during cycling, it is important to know the difference between medical and wellness tools. The Frontier X Plus is an FDA-cleared medical grade, prescription-based long term ECG monitor cleared for use in detecting atrial fibrillation, tachycardia and bradycardia. Cyclists use this when physicians want long term ECG recordings to evaluate cardiac trends.
The Frontier X2 is a wellness grade device that records ECG and heart rate data to help athletes understand effort, strain and recovery trends during training. This allows you to observe how your heart responds to long rides without needing patch-based systems or repeated adhesive monitors.
Both offer the ability to review heart behaviour during real rides, giving you a clearer picture of your own physiology and helping you adjust your training accordingly.
FAQs About Continuous ECG for Cyclists
1. Why is continuous ECG better than heart rate for long rides?
Heart rate only shows how fast your heart beats. Continuous ECG shows how well it beats. It helps you understand stress, rhythm patterns, fatigue and electrical changes that heart rate alone cannot reveal.
2. Can continuous ECG help me improve my cycling performance?
Yes. By matching ECG patterns to your effort, you can train more efficiently, manage fatigue better and avoid pushing into harmful overload.
3. Do I need a doctor to interpret my ECG every time?
Not necessarily. Athletes often use ECG devices to observe general training patterns. For medical concerns or unusual ECG findings, physicians can review the recordings and guide you professionally.
4. Is long term monitoring useful for recreational cyclists?
Absolutely. Even non competitive riders benefit from understanding how their heart reacts to heat, climbs and long endurance effort. It can help prevent overtraining and guide safer riding habits.
5. What is the main advantage of using ECG over wrist based heart trackers?
Wearable heart rate trackers rely on optical sensors which can become inaccurate during sweat, movement or vibration. ECG records electrical activity directly and remains stable during intense effort, providing more dependable insights.
As a runner, you know how crucial it is to balance training intensity with recovery. One powerful way to do this is by tracking your Heart Rate Variability (HRV). HRV, a dynamic measure of the time variation between heartbeats, provides valuable insights into your recovery status, readiness for training, and overall stress levels. Using HRV effectively can help you train smarter, avoid injuries, and optimize your running performance.
What is Heart Rate Variability (HRV)?
Heart Rate Variability is the variation in milliseconds between each heartbeat. It is controlled by your autonomic nervous system, which includes the sympathetic nervous system responsible for the fight-or-flight response, and the parasympathetic nervous system that drives rest and recovery. When your HRV is high, it signals that your body is well recovered and ready to perform. When your HRV is low, it can indicate fatigue, stress, or insufficient recovery, suggesting the need to dial back your training intensity.
Unlike a simple heart rate that measures beats per minute, HRV tells you how adaptable and resilient your heart and nervous system are to physical and mental stress. Monitoring HRV daily can empower you to make informed decisions about training and recovery tailored specifically to you.
Why Should Runners Track HRV?
For runners, HRV offers several benefits:
- Optimize Training: By observing your HRV trends, you can adjust training loads to maximize gains and avoid overtraining. High HRV means you can push harder; low HRV means focus on recovery.
- Prevent Injury and Burnout: Consistent low HRV readings may signal overtraining and heightened injury risk. Paying attention to this helps avoid muscle strains, bone stress, and irritations.
- Manage Stress Levels: HRV is sensitive to both physical stress like hard workouts and mental stress. Monitoring it helps you balance all stressors reducing burnout risk.
- Improve Recovery: Knowing how your nervous system rebounds after runs or workouts allows for smarter rest and sleep strategies, accelerating tissue repair and readiness.
In essence, HRV acts as a physiological dashboard, telling you if you need a rest day or a high-performance day. This is vital for injury prevention and sustained running progress.
Using Technology to Track HRV: Frontier X2
Tracking HRV has become easier and more accurate thanks to wearable technology, like the Frontier X2. The Frontier X2 is a wellness-grade heart monitor device that provides continuous HRV monitoring using advanced ECG technology. Unlike standard heart rate monitors or smartwatches, the Frontier X2 offers precise measurements of your cardiac activity with detailed data on HRV, breathing rate, strain, and heart rate zones.
What makes Frontier X2 unique for runners is that it not only records your HRV continuously during runs and rest but also provides real-time vibration alerts when your heart is out of your optimal zone. This helps prevent overstraining during workouts and promotes effective recovery by giving you immediate feedback.
You can also sync Frontier X2 easily with fitness apps for comprehensive heart health analysis and get AI-generated recommendations for your next workout based on your current physiological status. This turns your training into a highly personalized experience aimed at reducing injury risk and improving fitness faster.
The Role of Continuous Heart Monitoring
Unlike spot checks of heart rate or occasional ECGs, continuous heart monitoring tracks your heart’s behavior throughout the day and night. This comprehensive approach offers deeper insights into your autonomic nervous system balance and overall cardiovascular health.
For runners, continuous monitoring helps identify irregular heart rhythms early, detect signs of excessive strain, and allows timely interventions before adverse outcomes occur. It also highlights how well your body recovers during sleep, a critical factor since recovery takes place mostly when you rest.
Devices like the Frontier X2 enable this level of monitoring minus the need for bulky equipment or hospital visits. This empowers you to manage your health proactively within your training routine, ensuring safety and peak performance simultaneously.
Other Factors That Influence HRV and Recovery
While HRV gives you a clear window into your recovery, other lifestyle factors play key roles in heart health and running performance:
- Sleep Quality and Consistency: Poor or irregular sleep negatively impacts HRV and recovery. Aim for regular, quality sleep to maintain high HRV.
- Nutrition and Hydration: Inadequate fuel or dehydration stresses the body, reflected in lower HRV and higher injury risk.
- Stress Management: Emotional and mental stress elevate cortisol, reducing HRV. Techniques like mindfulness or meditation can improve your nervous system balance.
- Rest and Recovery Timing: Strategically planned rest days and cooldown routines allow your parasympathetic system to repair and strengthen.
In short, your recovery strategy should integrate HRV data with these lifestyle habits for the best results.
How to Use HRV to Optimize Recovery and Prevent Injury
- Track HRV Daily: Use devices like Frontier X2 to get accurate daily readings.
- Analyze Trends, Not Single Readings: Look for meaningful changes over weeks to adjust your training plan.
- Adjust Training Intensity: On low HRV days, reduce mileage or intensity and focus on active recovery or cross-training.
- Prioritize Sleep and Nutrition: Complement HRV insights with better sleep hygiene and adequate nutrition.
- Use Real-Time Alerts: During runs, real-time notification of heart rate zones and strain helps you stay within safe efforts.
- Consult Health Professionals if Needed: Continuous ECG data helps doctors intervene if abnormal rhythms or concerns arise.
FAQs
- What is heart rate variability and why is it important for runners?
Heart rate variability (HRV) measures the variation in time between heartbeats and reflects your body’s recovery and stress levels. For runners, understanding HRV helps optimize training, prevent overtraining injuries, and improve overall performance. - How can I measure my HRV effectively?
You can measure HRV accurately using devices like the Frontier X2, which offers continuous ECG-based monitoring and real-time insights into heart health, recovery, and stress. - Can HRV prevent running injuries?
Yes, monitoring HRV can reveal if you are under excessive stress or fatigue, helping you adjust workouts before injuries like muscle strains or bone stress occur. - What role does continuous heart monitoring play for runners?
Continuous heart monitoring, provided by devices like Frontier X2, detects irregular heart activity, tracks recovery, and provides ongoing feedback to keep training safe and effective. - How should I adjust my training based on HRV readings?
Higher HRV indicates readiness for hard training, while lower HRV suggests you should prioritize rest and light activity. Adjusting your training intensity based on HRV can optimize performance and minimize injury risk.
Final Thoughts
As a runner wanting to perform your best while staying injury-free, integrating Heart Rate Variability monitoring into your routine is a game-changer. Devices like the Frontier X2 deliver continuous, precise heart insights that help you understand your recovery needs and optimize training loads. Combining HRV data with smart lifestyle choices like quality sleep, nutrition, and stress management will keep you running longer, stronger, and healthier.
Stay connected to your body’s signals with daily HRV monitoring – your heart will thank you for it.
You walk into the gym with one goal in mind. To get stronger. To push harder. To level up. Whether you are lifting your first barbell or chasing elite-level performance, the desire to improve is universal.
But there is a fine line that separates smart progress from silent overload. That line is where training load and heart strain intersect.
You may feel sore, tired, or breathless after a hard session. That is expected. But what is happening inside your heart during those intense sets is something most people never truly understand. And that lack of awareness is often what holds athletes back from real breakthroughs or pushes them toward burnout and injury.
If you want to train like an elite athlete, you must start thinking like one. That means learning how to balance effort with recovery and listening to your heart just as carefully as your muscles.
What Training Load Really Means for Your Body
Training load is more than how heavy you lift or how long you train. It is the total stress placed on your body from:
- Volume
- Intensity
- Frequency
- Recovery demands
Every squat, sprint, deadlift, and conditioning circuit adds to your internal load.
Two people can follow the same workout plan but experience very different strains. One recovers quickly and adapts. The other stays fatigued, struggles to improve, and risks injury. The difference is not willpower. It is how their body handles stress.
Your muscles are not the only systems that feel this load. Your heart responds instantly to every change in effort. As intensity rises, your heart rate rises. As fatigue accumulates, recovery slows. Over time, repeated overload without enough recovery can quietly strain your cardiovascular system.
This is why heart strain has become a growing focus in modern performance training.
What Is Heart Strain in the Gym Context
Heart strain is not a medical diagnosis in the gym setting. It is a performance concept. It refers to how hard your heart is working during training and how well it recovers afterward.
You experience heart strain when your heart is forced to sustain high effort for long periods without enough rest. This often happens with:
• High volume circuit training
• Excessive high-intensity intervals
• Long sessions with poor recovery
• Training through chronic fatigue
• Stacking strength and cardio without planning
At first, your fitness improves. Then your progress stalls. Sleep worsens. Motivation drops. Heart rate remains elevated. You feel flat even on light days. These are early warning signs that your training load may be outweighing your ability to recover.
Elite athletes do not train harder than everyone else every day. They train smarter.
Why Balancing Training Load Separates Amateurs From Elites
Amateurs chase exhaustion. Elites chase efficiency.
An amateur judges success by how destroyed they feel after a session. An elite athlete judges success by how well they can repeat high-quality work day after day without burnout.
The key difference is load management. Elite athletes:
• Adjust training intensity based on recovery, not emotion
• Understand that progress comes from adaptation, not just effort
• Train with the goal to perform tomorrow, not just survive today
If you want to move from amateur to elite, thinking inside the gym, you must shift your mindset in three key ways:
• You train for long-term consistency, not short-term punishment
• You respect recovery as much as effort
• You use data, not ego, to guide intensity
This is where heart-based training insights become incredibly powerful.
How Your Heart Reveals Training Readiness
Your heart responds to stress faster than any muscle group. It reacts to:
• Physical load
• Sleep quality
• Hydration
• Mental stress
• Poor nutrition
That makes it one of the best mirrors of your true readiness.
When your training load is balanced:
- Your heart rate rises proportionally with effort
• Your recovery between sets stays efficient
• Your resting heart rate remains stable
• Your heart rate variability trends remain healthy
When training load exceeds recovery:
- Heart rate stays elevated longer
• Recovery between sets slows
• Sleep heart rate increases
• Daily fatigue becomes persistent
You may still be lifting the same weights. But internally, your system is under strain. This is why top-level strength coaches and sports scientists now emphasize heart data as a core performance signal, not just an endurance metric.
The Silent Risk of Ignoring Heart Strain
Pushing hard feels productive. But ignoring heart strain carries long-term risks.
Chronic overload can contribute to:
• Reduced training tolerance
• Overtraining syndrome
• Increased injury risk
• Hormonal disruption
• Cardiovascular stress accumulation
Most gym athletes assume heart issues only affect endurance athletes. That is no longer true. Modern high intensity gym programming places sustained stress on the heart especially during long circuits and conditioning blocks layered onto heavy lifting.
You do not need to fear hard training. You only need to learn when hard becomes harmful.
How Smarter Load Management Improves Performance
When you manage training load correctly, your results improve across every metric:
• Strength increases faster
• Recovery improves
• Fat loss becomes more consistent
• Sleep quality improves
• Mental focus sharpens
• Injury risk drops
You stop chasing fatigue and start chasing repeatable performance. The goal is not to avoid strain. The goal is to apply it with precision.
The Role of Long Term Heart Monitors in Measuring Training Load During Exercise
Modern athletes now have the ability to observe how their heart responds to training beyond the gym floor.
Medical grade tools like the Frontier X Plus support long term ECG monitoring for clinical level heart rhythm and rate tracking. Wellness grade devices like the Frontier X2 allow athletes to record ECG and heart rate data for fitness and wellness insights. Together they help you and your physician observe how your heart behaves over extended periods of training, stress recovery and daily activity.
These tools do not replace medical care. They support trend awareness. They help identify how intense sessions influence your heart over time. They also help you recognize when your system is adapting well and when fatigue patterns may require smarter recovery decisions.
This visibility helps bridge the gap between effort and safety for serious gym athletes.
Signs You Need to Rebalance Your Training Load
You may need better load management if you notice:
• Persistent elevated heart rate at rest
• Poor sleep despite heavy fatigue
• Loss of motivation to train
• Reduced performance at the same weights
• Frequent soreness that never fully resolves
• Longer recovery between sets
These signs do not mean you are weak. They mean your system is asking for smarter structure.
How to Balance Training Load Like an Elite Athlete
You do not need a professional team to apply elite principles. Start with these fundamentals.
1. Plan Variation Into Your Week
Alternate heavy and lighter days. Do not stack maximal strength high volume conditioning and poor sleep together repeatedly.
2. Respect Recovery Metrics
Watch how quickly your heart rate falls after intense sets. Faster recovery often signals better conditioning and fresher readiness.
3. Train With Intent Not Emotion
Not every session needs to be a battle. Some days are for building. Some days are for restoration.
4. Eat and Hydrate for Performance
Low fuel states elevate heart strain during training. Under-eating makes hard sessions harder on your heart.
5. Sleep Is Non Negotiable
Lack of sleep raises resting heart rate and depresses recovery. No program can out train poor sleep.
From Gym Warrior to High Performance Thinker
Moving from amateur to elite is not about lifting the heaviest weight once. It is about lifting well for years without breakdown.
Your heart is not just a survival organ. It is a performance engine. Every rep you do moves through it. Every recovery period depends on it.
When you learn to respect heart strain instead of ignoring it you unlock a higher tier of training intelligence. You gain control over your progress rather than relying on brute force.
The Long Term Payoff of Smart Heart Aware Training
Athletes who learn to balance load and heart strain experience:
• More consistent strength gains
• Fewer forced layoffs due to burnout
• Better endurance during gym work
• Improved metabolic conditioning
• Higher confidence in pushing limits safely
You stop guessing when to push and when to pull back. You start knowing.
That transition is what separates recreational effort from elite preparation.
Final Takeaway
Your muscles adapt in weeks. Your nervous system adapts in months. Your heart carries the load every second.
If you want to train harder without burning out. If you want to lift heavier without breaking down. If you want to move from amateur mindset to elite execution.
You must learn to balance training load with heart strain.
Your progress does not depend on how hard you suffer in one session. It depends on how well you recover and repeat high quality effort over time.
FAQs
-
What is training load in gym workouts
Training load refers to the combined stress from workout intensity, volume frequency and recovery demands placed on your body.
-
Can heavy gym training strain the heart
High intensity and long duration gym sessions can increase cardiovascular strain especially when recovery is inadequate.
-
How do I know if my heart is overworked from training
Signs include elevated resting heart rate, slow recovery fatigue, poor sleep and declining performance.
-
Is heart monitoring useful for strength training
Yes heart data helps you understand recovery training readiness and internal stress even during resistance based training.
-
How does ECG monitoring support athlete safety
Long term ECG monitoring helps track heart rhythm and rate trends over time so athletes and physicians can observe how training stress influences the heart.
In the world of athletic performance, the focus is often on heart rate, pace, and power. But a metric that’s gaining traction for how it affects recovery, fatigue, and injury risk is body shock – the mechanical impact your body experiences with every foot strike, jump or hard movement. Understanding how body shock contributes to muscle fatigue, and how it integrates with cardiovascular strain and recovery, can help athletes train smarter and stay healthier over time.
What Is Body Shock?
Monitoring your Body Shock to analyse the impact of running surfaces, gear, form changes or fatigue, helps prevent injuries during high impact activities.”
In practical terms, high body shock means your musculoskeletal system (muscles, tendons, bones) is absorbing greater forces. Over time, unless recovery is adequate or the training is adapted, these forces can lead to micro-trauma, fatigue, delayed recovery and injury risk.
How Body Shock Enables Muscle Fatigue
Muscle fatigue isn’t just about working hard – it’s about the accumulation of forces and the body’s capacity to absorb, dissipate, and recover from them. Here’s how body shock ties into that:
- Impact Forces and Mechanical Load
Athletes who land heavily, run on hard surfaces, increase stride length aggressively, or train under fatigue often gang up on higher body shock values. This means each step has a higher load travelling through the body. Over time, muscles must work harder to stabilise the joints and absorb the forces, leading to earlier onset of fatigue. - Fatigue Alters Mechanics
When muscles are fatigued, coordination drops. This often leads to poorer landing technique (higher vertical oscillation, lower cadence in runners) or stiffer limb deceleration. Higher body shock = higher load per step = more mechanical stress on muscles already on edge. The cycle accelerates. - Cardiovascular Strain and Muscular Exhaustion
The Frontier X2 pairs body shock with heart metrics such as heart rate, strain, HRV and breathing rate. When body shock is high, the cardiovascular system must support more muscular loading and metabolic demand. The device defines “Heart strain” as a measurement based on the ST-segment deviation recorded by the Frontier X2 device from the CC5 Lead position. This deviation could be due to a variety of reasons, including oxygen deprivation to a part of your heart, electrolyte imbalance and conduction defects. When your heart is working harder to keep up with mechanical load plus fatigue, muscle fatigue is exacerbated and recovery slowed. - Recovery Capacity and Overtraining Risk
Body shock monitoring lets you see when your body’s impact load is climbing due to fatigue, surface changes, or form breakdown. “High Body Shock, especially during running, can be associated with a greater risk of injuries such as stress fractures.” Fatigued muscles cannot absorb forces optimally, elevating body shock, which then further fatigues muscles – a negative feedback loop.
Why This Matters for Athletic Performance
For athletes – from weekend warriors to elite competitors – the ability to control mechanical stress, monitor recovery and reduce fatigue is critical. Here’s why body shock matters:
- Injury Prevention: High shock loads are linked to stress fractures, soft-tissue overuse injuries and muscle strain. Monitoring body shock helps you identify when training load and impact exposure are too high.
- Performance Sustainability: Being able to perform high volumes and intensities without accumulating fatigue is partly down to how well your body handles mechanical load. Lower body shock for the same volume = better efficiency.
- Recovery Optimisation: If your body’s accumulated mechanical burden is high, your recovery needs increase. Tracking body shock helps gauge when your body needs lighter training or active recovery to reset fatigue.
- Form and Technique Feedback: Monitoring impact forces gives you objective insight into how your running/cycling/etc. mechanics change over time – often due to fatigue, poor surface or inappropriate gear. Correcting these early stops fatigue creeping in.
- Training Load Balancing: Many devices track heart rate or pace, but few integrate mechanical shock with cardiovascular strain to measure total load. Body shock adds a dimension of biomechanical load that complements physiological load.
How the Frontier X2 Supports Body Shock Monitoring
The Frontier X2 is designed from a wellness and performance perspective – not a medical device – yet it integrates long-term ECG, body shock, training load and strain monitoring in one wearable. Some of its relevant features:
- Measures Body Shock in real-time during running, HIIT and high-impact activities.
- Provides Strain monitoring which quantifies cardiovascular stress (oxygen demand on heart) during different activities.
- Long-term ECG and heart monitoring during exercise: precise heart rate + HRV + rhythm charts to understand recovery and fatigue.
- Training Load and readiness metrics: Recognises when the sum of mechanical load + cardiovascular load is too high and helps you plan recovery.
- Surface, gear and mechanical inputs: Helps you assess how training on road vs trail, changes in shoes, or fatigued form contribute to higher shock loads.
From a wellness viewpoint, this means you don’t have to guess when your training is pushing your body into a fatigue-trap. Instead you use objective data – mechanical shock + heart strain + readiness – to guide your sessions and recovery.
Practical Steps to Mitigate Muscle Fatigue via Body Shock Monitoring
Here are actionable suggestions for athletes:
- Monitor Body Shock Trends
Use your device’s dashboard to monitor how your body shock values change over days, weeks or sessions. Rising values may indicate fatigue, form change or inappropriate surface/gears. - Watch For the Strain & HRV Indicators
When strain or HRV begin to shift unfavourably at the same time body shock is high, it’s a warning sign: your body is under mechanical and cardiovascular load. Dial back volume/intensity and prioritise recovery. - Adapt Training Surfaces and Gear
If body shock spikes when you switch from grass to concrete or from cushioning shoes to minimal ones, adjust accordingly. The device supports this by tracking body shock by surface. - Prioritise Recovery Sessions
If your body shock remains elevated across sessions, include low-impact alternatives (cycling, swimming), strength work (especially hips/legs/core), and mobility to reduce mechanical load. - Form Check and Technique Focus
Fatigue often alters form. Use body shock data as feedback – if values shift upwards for the same speed/volume, you might be landing harder or moving differently. Incorporate drills to improve mechanics. - Balance Training Load with Mechanical Load
Traditional training load metrics (volume, intensity, heart rate) are important – but combining them with body shock gives a fuller load picture. Use both to avoid overtraining.
By focusing on the under-explored link between mechanical impact (body shock) and muscle fatigue, and by showcasing the Frontier X2’s wellness-grade monitoring capabilities, this blog positions itself as a valuable resource for athletes and fitness-focused readers looking to optimise training, recovery and injury prevention.
FAQs
Q1: What is body shock in athletic training?
Body shock refers to the mechanical stress or impact forces transmitted through your body during activities such as running or jumping. Measuring body shock helps understand how training load and impact affect muscles, joints and fatigue.
Q2: How does body shock contribute to muscle fatigue?
High body shock means greater forces per movement which require your muscles and joints to absorb more load. Over time, this accelerates fatigue, reduces efficiency, alters form and increases injury risk.
Q3: Can athletes monitor mechanical load in real-time?
Yes. Modern wearables like the Frontier X2 integrate sensors that measure body shock (impact forces), heart rate, strain and training load in real time – providing actionable data during workouts.
Q4: What training adjustments should I make when body shock values increase?
Consider reducing high-impact activity volume, switching to softer surfaces, increasing recovery sessions, improving form/technique, and incorporating strength/mobility work to absorb impact more efficiently.
Q5: Is body shock important only for runners?
No. While body shock is often discussed in running, the concept applies to any high-impact or plyometric activity (jumping, HIIT, change of direction sports). The key is how your body absorbs load and what recovery strategy you use.