Home » Heart Health » Angina Explained: What Your Chest Pain Might Be Telling You

Understanding Angina: A Warning Sign from the Heart
Chest pain is one of the most alarming symptoms anyone can experience. While not every instance of chest pain means a heart attack, it should never be ignored – especially when it’s angina.
Angina pectoris, commonly called angina, is not a disease itself but a symptom of underlying heart disease, typically coronary artery disease (CAD). It occurs when the heart muscle doesn’t get enough oxygen-rich blood, often due to narrowed or blocked coronary arteries.
When the oxygen supply is insufficient, the heart sends distress signals in the form of chest discomfort, pressure, or pain. Recognizing and addressing these signs early can be the key to preventing a serious cardiac event.
What Does Angina Feel Like?
Angina pain is often described as:
- Tightness or pressure in the chest
- Burning, squeezing, heaviness, or even shooting or stabbing discomfort that may radiate to the jaw, neck, shoulders, arms, or back. This discomfort may not only spread to these areas but can also originate from them. However, individuals with diabetic autonomic neuropathy may not experience any of these sensations due to reduced pain perception.
- A feeling of fullness or discomfort, especially during exertion
- Shortness of breath, nausea, or fatigue are common, particularly in women and older adults. However, some women, especially older women, may not experience these typical symptoms. Instead, they may present with atypical signs such as subtle changes in cognitive function or symptoms that mimic other conditions, like a urinary tract infection.
The discomfort usually lasts a few minutes and eases with rest or medication like nitroglycerin. However, persistent or worsening pain should always be evaluated immediately – as it could indicate a heart attack.
Types of Angina
Angina is classified into several types, each reflecting a different underlying mechanism or risk level:
1. Stable Angina
The most common form, stable angina occurs predictably with physical exertion, stress, or cold weather and subsides with rest. It signals partial blockage of coronary arteries but indicates a chronic, manageable condition if treated properly.
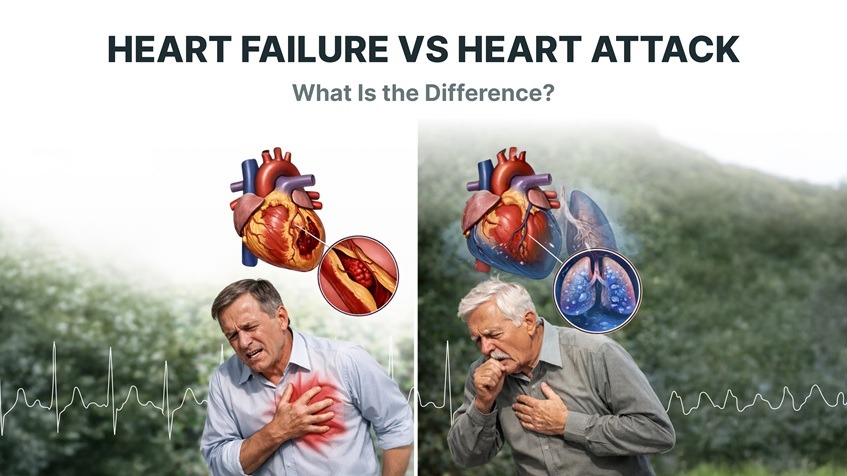
2. Unstable Angina
This is a medical emergency. Unstable angina occurs at rest or with minimal exertion and may last longer than a few minutes. It often means a plaque rupture or clot has significantly reduced blood flow – a warning sign of an impending heart attack.
3. Variant (Prinzmetal’s) Angina
Caused by spasms in the coronary arteries rather than plaque buildup, this form of angina can occur at rest, often at night or early morning. It may cause severe pain and temporary ECG changes but usually resolves with vasodilators.
4. Microvascular Angina
Sometimes referred to as cardiac syndrome X, this type involves dysfunction of the small blood vessels of the heart. It is more common in women, and traditional angiograms may appear normal despite ongoing ischemia (low blood flow).
Common Causes and Risk Factors for Angina
Angina arises primarily due to reduced coronary blood flow, but several factors increase the risk:
- Atherosclerosis (plaque buildup in arteries)
- High blood pressure (hypertension)
- High cholesterol levels
- Diabetes mellitus
- Obesity and sedentary lifestyle
- Smoking
- Chronic stress
- Family history of heart disease
Each of these contributes to damage or narrowing of the coronary arteries, making it harder for the heart to receive sufficient oxygen during times of increased demand.
When Chest Pain Should Not Be Ignored
While not every chest discomfort is heart-related, angina-like symptoms should always prompt evaluation. Seek immediate help if:
- Chest pain occurs at rest or during minimal activity
- Pain spreads to the arms, back, neck, or jaw
- It is accompanied by sweating, nausea, or breathlessness
- The discomfort persists for more than 5–10 minutes despite rest
In these cases, call emergency services – it could be unstable angina or a heart attack requiring urgent medical care.
Diagnosis: How Doctors Identify Angina
Diagnosing angina involves a combination of clinical assessment, ECG monitoring, and imaging tests. Common diagnostic approaches include:
- Electrocardiogram (ECG): Detects abnormalities in heart rhythm and ischemic changes.
- Stress Test: Monitors ECG during physical exertion to assess blood flow under stress.
- Continuous ECG Monitoring: Tracks real-time heart rhythm patterns and transient ischemic changes that may occur outside of clinical settings.
- Echocardiogram: Evaluates heart function and blood flow.
- Coronary Angiography (CT and invasive): Visualizes arterial blockages through X-ray imaging.
Continuous ECG or wearable heart monitors can detect short-lived ischemic episodes that may go unnoticed in routine clinic tests, providing deeper insights into daily heart performance.
Treatment for Angina: Restoring Blood Flow and Relieving Pain
The goal of angina treatment is to improve blood flow to the heart, reduce symptoms, and prevent future cardiac events.
Lifestyle Changes
- Quit smoking and limit alcohol intake
- Adopt a heart-healthy diet rich in fruits, vegetables, and omega-3s
- Exercise regularly, under medical supervision
- Manage stress and maintain healthy body weight
- Control diabetes, cholesterol, and blood pressure
Medications
(Important: The medications listed below are for general awareness only. Treatment should always be determined by a qualified physician. Never start, stop, or adjust any medication without consulting your healthcare provider.)
- Nitrates (e.g., Nitroglycerin): Dilate blood vessels to improve blood flow and relieve pain
- Beta-blockers: Slow the heart rate, reducing oxygen demand
- Calcium channel blockers: Relax arteries and lower blood pressure
- Antiplatelet agents (e.g., Aspirin): Prevent clot formation
- Statins: Lower cholesterol and stabilize arterial plaques
Medical Procedures
If medication alone isn’t enough, doctors may recommend:
- Angioplasty and Stent Placement: To open narrowed arteries
- Coronary Artery Bypass Grafting (CABG): To reroute blood flow around blockages
Long-Term ECG Monitoring and the Role of Frontier X Plus
For individuals experiencing recurrent chest discomfort or suspected angina episodes, long-term ECG monitoring provides valuable insights into heart rhythm patterns.
Devices like Frontier X Plus allow users to record extended ECG waveforms and heart rate, with the option for live viewing during daily activities or workouts. This enables clinicians and users to understand how the heart responds under stress, exertion, and rest.
Long-term ECG monitoring can:
- Capture transient changes in heart rhythm that short ECGs may miss
- Track heart rate variability and rhythm patterns
- Help clinicians correlate symptoms, such as chest discomfort, with recorded ECG trends
For patients with stable angina or undergoing post-treatment follow-up, Frontier X Plus provides a non-invasive way to observe ongoing heart activity in relation to daily lifestyle, supporting continuous evaluation and proactive heart health management.
Living with Angina: Managing and Preventing Recurrence
Angina can be a lifelong condition, but it doesn’t have to limit your life. The key is vigilant management and consistent monitoring:
- Follow your medication regimen carefully.
- Track your heart rate and ECG using advanced wearables.
- Maintain regular follow-ups with your cardiologist.
- Stay attentive to warning signs and avoid triggers like overexertion and emotional stress.
With early detection and smart monitoring, most patients with angina can lead active, fulfilling lives while reducing their risk of heart attack.
Key Takeaways
- Angina is chest pain caused by reduced blood flow to the heart.
- It signals underlying coronary artery disease and can precede a heart attack.
- Stable angina occurs with exertion; unstable angina can appear at rest and is an emergency.
- Diagnosis involves ECG, stress testing, and sometimes angiography.
- Long-term ECG monitoring devices, such as Frontier X Plus, record extended heart rhythm data, allowing clinicians and users to observe transient changes in cardiac activity and support ongoing heart health evaluation.
FAQs
Q1: What causes angina chest pain?
Angina occurs when reduced blood flow through narrowed coronary arteries limits oxygen supply to the heart muscle, causing pain or discomfort.
Q2: How do I know if my chest pain is angina or a heart attack?
Angina usually improves with rest or medication, while heart attack pain is more severe, lasts longer, and may include nausea, sweating, and breathlessness. Always seek emergency help if uncertain.
Q3: What is the treatment for angina?
Treatment includes lifestyle changes, medications like nitrates or beta-blockers, and in severe cases, angioplasty or bypass surgery to restore blood flow.
Q4: Can angina be detected on ECG?
Yes. Angina-related ischemia often shows ST-segment or T-wave changes on ECG. Continuous ECG monitoring can detect transient episodes missed in short tests.
Q5: How can continuous ECG monitoring help angina patients?
Long-term ECG devices like the Frontier X Plus record continuous heart rhythm data and allow live viewing of ECG signals. This enables users and clinicians to review heart activity during episodes of chest discomfort and understand how the heart responds to exertion or stress, supporting further clinical evaluation and personalized management.
Related Posts
You might also like
-

Featured Articles
- Why Body Shock Monitoring Is Crucial for Every AthleteJanuary 7, 2026
- Frontier X2 vs Smart Ring: Which Wellness Tracker Knows...November 28, 2025
- The ROI of Investing in Frontier X2 With HSA/FSANovember 21, 2025
- Why Body Shock Monitoring Is Crucial for Every Athlete
CATEGORIES
POPULAR POSTS
- How Cold Weather Can Affect Heart Rhythm Disorders
- Can Overtraining Increase Your Risk of Heart Rhythm Issues
- Frontier X Plus Versus ECG Patches: Which Is Right for Long-Term Heart Rhythm Monitoring?
- Why Sudden Heart Rate Spikes During Exercise Should Not Be Ignored
- Frontier X Plus vs. Handheld Device: Which ECG Monitoring Approach Is Right for You?
-
Follow us on
Top Searches for Heart Health
Top Searches for AFib
Frontier X2 Smart Heart Devices
Top Searches for Heart Rate
VISUAL STORIES