Running long distances is often seen as the epitome of physical fitness. From marathons to ultramarathons, endurance athletes are celebrated for their stamina, discipline, and cardiovascular health. However, emerging research and clinical cases reveal a more nuanced picture – long-term endurance exercise, especially at extreme levels, may come with potential cardiac risks.
Here, we’ll explore the various cardiac risks associated with long-distance running, highlight the symptoms to watch for, and discuss how monitoring long-term ECG with tools like the FDA cleared Frontier X Plus and wellness-based Frontier X2 can play a pivotal role in early detection and prevention.
Understanding the Athletic Heart vs. a Compromised Heart
Long-distance running induces structural and functional changes in the heart. Often referred to as “athlete’s heart,” these adaptations include a slower resting heart rate, enlarged cardiac chambers, and increased stroke volume. These changes are usually benign.
But how do you differentiate healthy heart adaptations from pathological changes that could lead to serious heart conditions?
Common Misconception:
A low resting heart rate and enlarged heart on imaging aren’t always safe. In some cases, they may mask or resemble signs of underlying cardiac disease.
Cardiac Risks in Long Distance Runners
1. Atrial Fibrillation (AFib)
One of the most well-documented conditions among endurance athletes is atrial fibrillation, a type of irregular heart rhythm. Studies suggest that long-distance runners are at an increased risk of AFib due to chronic volume overload and atrial stretching.
Warning Signs:
- Palpitations
- Dizziness or fainting
- Fatigue despite regular training
- Irregular pulse
2. Myocardial Fibrosis
Chronic extreme endurance exercise has been associated with scarring of the heart muscle, particularly the right ventricle. Over time, this can lead to arrhythmias and even heart failure. Myocardial fibrosis often goes undetected in routine cardiac screenings.
3. Right Ventricular Dysfunction
Unlike strength training, long-distance running places significant load on the right ventricle. Repeated stress can result in transient or even permanent dysfunction, which increases the risk of ventricular tachycardia and other dangerous arrhythmias.
4. Coronary Artery Calcification (CAC)
Surprisingly, even in athletes with a low traditional cardiac risk profile, studies have found elevated levels of coronary artery calcium, a marker for atherosclerosis. These plaques may not always be stable and could lead to cardiac events during or after endurance events.
5. Sudden Cardiac Arrest (SCA)
Although rare, sudden cardiac arrest in endurance athletes usually occurs due to undiagnosed conditions like:
- Hypertrophic cardiomyopathy
- Arrhythmogenic right ventricular cardiomyopathy
- Coronary anomalies
Most of these conditions are silent and may only be revealed through advanced monitoring techniques.
6. Exertional Hypertension
Long-distance runners may experience significant blood pressure spikes during races or intense training. Over time, this can lead to left ventricular hypertrophy and increased risk of stroke and heart failure.
Why Symptoms May Be Missed
Many runners pride themselves on high pain tolerance and are conditioned to ignore minor symptoms. However, subtle signs like:
- Palpitations at night
- Shortness of breath despite fitness
- Exercise intolerance
- Elevated heart rate at rest or during sleep
… could indicate something more serious than overtraining.
The Role of Long-Term ECG Monitoring in Runners
Traditional screening methods like resting ECGs or short-duration Holter exams may not always reflect how the heart behaves during exertion or recovery.
That’s where chest-strap-based, long-term ECG devices such as the wellness-focused Frontier X2 come in. These personal ECG tools record heart data continuously, providing a comprehensive view of cardiac activity during daily routines, exercise, and rest.
Key Benefits for Runners:
- Record ECG during training and rest, allowing their healthcare providers to review potential irregularities such as unusual beats or rhythm patterns.
- Track heart rate variability (HRV) and physiological strain to understand training intensity and recovery trends.
- Deliver high-resolution ECG-quality data that can support clinical review or research use when appropriately supervised by healthcare professionals.
- Provide insights into rhythm patterns to help users and clinicians discuss whether observed changes may warrant further evaluation.
- Capture heart rate trends during sleep and recovery for a complete picture of cardiac performance.
- Measure body shock levels, reflecting the mechanical stress your body experiences with every stride – a valuable indicator for optimizing running form and preventing overtraining.
Frontier X2 offers a non-invasive, patchless, and sweat-resistant option – ideal for runners who want to train smarter and safer.
When Should Long Distance Runners Be Concerned?
Here are a few scenarios when runners should consider a deeper cardiac evaluation:
- Unexplained fatigue or reduced performance
- Heart palpitations during or after exercise
- Family history of sudden cardiac death
- Dizziness or fainting episodes
- Elevated heart rate at rest or while sleeping
- Chest discomfort unrelated to effort
In such cases, a long-term ECG monitor can provide crucial insight that a regular smartwatch or fitness tracker simply cannot.
Prevention: Running with Heart-Smart Awareness
While the risks exist, it doesn’t mean athletes should stop running. Instead, awareness and proactive heart monitoring can mitigate risks significantly.
Pro Tips for Long Distance Runners:
- Get screened: Periodic cardiac checkups with ECG and echocardiography
- Hydrate and fuel smartly: Avoid electrolyte imbalance, especially in long races
- Track your heart: Use clinically validated ECG monitors, especially during high-intensity training blocks
- Listen to your body: Fatigue, dizziness, or irregular heartbeat shouldn’t be ignored
- Limit excessive volume: Allow proper rest periods and consider de-training phases to avoid chronic stress
Final Thoughts
The athletic lifestyle offers immense cardiovascular benefits, but ultra-endurance training is not without its risks. What’s important is not to fear these risks – but to understand and manage them effectively.
By leveraging tools like long-term ECG monitors, runners can go the extra mile safely, with real-time insights into how their heart is responding to stress, exertion, and recovery.
Remember:
It’s not just about how far or fast you run – it’s about how well your heart handles the journey.
FAQs
1: Can long-distance running cause heart problems?
Yes. Intense, prolonged running can sometimes lead to arrhythmias, heart enlargement, or scarring in some individuals.
2: What are the early signs of heart issues in runners?
Shortness of breath, chest pain, dizziness, or irregular heartbeat – especially during or after exercise – can be warning signs.
3: How can runners lower their risk of cardiac events?
Regular check-ups, smart training, hydration, and using a continuous ECG monitor help reduce risk.
4: Is heart rate monitoring enough for endurance athletes?
Not always. Heart rate tracking misses arrhythmias – continuous ECG offers deeper insight into heart rhythm.
5: Does endurance running increase the risk of AFib?
Yes, over time. Long-term high-intensity training may increase the risk of AFib, especially in older male athletes.
In the age of personalized health tech, more people are relying on wearable devices to track fitness, sleep, and heart metrics. But when it comes to continuously monitoring your heart, understanding patterns in your heart rhythm during stress or sleep, or recording data that may reveal potential irregularities, a more advanced ECG monitor like the chest strap-based, patchless Frontier X2 offers continuous recording for detailed review.
Let’s break down the differences between the Frontier X2 and smartwatches, and explore which one offers deeper insights into your cardiovascular health.
Smartwatches: Great for Fitness, Limited for Heart Health
1. What They Measure
Most smartwatches like the Apple Watch, Fitbit, or Garmin offer:
- Spot ECG recordings (typically 30 seconds)
- Resting heart rate
- Heart rate variability (HRV)
- Basic sleep tracking
- Blood oxygen (SpO2)
They’re optimized for convenience and lifestyle metrics – but not continuous monitoring. Their ECG function is usually on-demand and only captures a snap shot of your heart rhythm.
2. Where They Fall Short
Smartwatches often miss intermittent or exertion-related heart issues:
- They don’t record ECG continuously.
- They rely heavily on optical sensors, which struggle during exercise due to sweat and motion.
- AFib and other arrhythmias that come and go may not be caught in short ECG recordings.
- They aren’t designed to detect P waves, which are critical in differentiating types of arrhythmias.
In essence, if your heart condition is subtle, or only shows up under stress or during sleep, your smartwatch might not catch it.
Frontier X2: Built for Real Heart Monitoring
The Frontier X2 is designed for people who want more than just a fitness overview – they want detailed heart rhythm tracking.
1. Continuous Monitoring
Unlike smartwatches, the Frontier X2:
- Records single-lead ECG continuously for up to 24 hours.
- Provides P wave visibility, which helps physicians in differentiating heart rhythm patterns.
- Captures ECG data continuously, without needing to press a button.
This makes it ideal for individuals who experience intermittent symptoms or want long-duration heart monitoring, especially during sleep or exercise. The recorded ECGs can then be reviewed by a clinician for potential irregularities such as AF, bradycardia, or tachycardia..
2. Monitoring Body Shock and Strain
The Frontier X2 goes beyond the heart. It also tracks:
- Body Shock: The impact force when your body hits the ground, especially during running or high-impact workouts.
- Breathing Rate: Useful for understanding cardiac stress and sleep-related breathing irregularities like sleep apnea.
- Heart Rate and HRV: Continuously measured even during high motion activities, providing more accurate data than optical sensors.
Sleep and Heart Health: A Hidden Risk
One of the most critical times for your heart is while you’re sleeping. Conditions such as sleep apnea, nocturnal AFib, bradycardia, or nighttime heart palpitations may occur during this time.
Unlike most smartwatches, Frontier X2 continuously records a full night’s ECG data, providing detailed heart information. This recorded data can then be reviewed by a clinician for potential irregularities or sleep-related cardiac stress
Who Might Benefit From Frontier X2 Compared to a Smartwatch?
1. Athletes and Fitness Enthusiasts
If you’re pushing your limits with high-intensity training or long-distance runs, Frontier X2 helps you monitor strain, body shock, and recovery, reducing the risk of overtraining or cardiac events during workouts.
2. People with Cardiac Conditions
Those who wish to record extended-duration ECG data for clinician review can benefit from continuous, chest-based monitoring. Unlike short, optical heart rate readouts, continuous ECG recording offers a clearer picture of heart rhythm patterns during daily activities and rest. Such insights can support ongoing clinical evaluation, treatment discussions, and a better understanding of how the heart responds over time.
3. Concerned Individuals with Unexplained Symptoms
If you’ve felt:
- Dizziness or fainting
- Palpitations or skipped beats
- Fatigue after minor exertion
…and want to get to the root cause, Frontier X2 can record what a smartwatch might miss.
Data You Can Trust – and Share
Smartwatches may give you a fitness snapshot, but Frontier X2 produces a full heart health report that:
- Can be shared with your cardiologist
- Provides continuous ECG trend data for clinician interpretation and review
- Provides live ECG streaming to a remote reviewer
- Is stored securely for later review or comparative analysis
This makes Frontier X2 not only a personal health device but also a bridge to better health management and physician-guided decision-making.
Smartwatch + Frontier X2: Can They Work Together?
Absolutely. Think of the Frontier X2 as your wellness-grade ECG monitor, and your smartwatch as your lifestyle dashboard.
Use your smartwatch for:
- Daily activity tracking
- Sleep routines
- Calorie burn and steps
And bring in the Frontier X2 when you need deeper insight – during training, overnight sleep, periods of unexplained symptoms, or when your doctor recommends monitoring.
What the Science Says
Research shows that intermittent ECGs miss up to 50% of arrhythmic episodes, especially when they’re brief or occur during sleep or exercise. This means your smartwatch might say “all’s good” while a silent AFib episode passes unnoticed.
Frontier X2’s long-term monitoring closes that gap – delivering ECG quality on par with traditional Holter monitors, but without the wires, patches, or hospital visits.
Conclusion: Which One Understands Your Heart?
If your goal is to track fitness and stay active, a smartwatch may be enough.
But if you want to:
- Record detailed ECG data continuously for deeper insights
- Identify lifestyle patterns that may correlate with sensations like palpitations or stress
- Monitor heart rate trends during sleep and recovery
- Access actionable ECG information that your clinician can review and interpret
- Take a proactive approach to understanding your heart’s performance
…then the Frontier X2 is the clear winner.
It’s the difference between watching your heart and truly understanding it.
Coronary artery disease (CAD) – also called ischemic heart disease or atherosclerotic heart disease – is the most common type of cardiovascular disease worldwide and a leading cause of death. It occurs when the coronary arteries that supply blood to the heart muscle become narrowed or blocked due to the buildup of plaque (fat, cholesterol, and other substances). This process, called atherosclerosis, can progress silently for years before showing symptoms.
The good news? If CAD is detected early, it can be treated and managed effectively, reducing the risk of heart attacks, heart failure, and other serious complications.
This article explains what CAD is, its warning signs, treatment options, and how patchless, chest-strap-based, long-term ECG monitors can support early detection and ongoing monitoring for people at risk.
Understanding Coronary Artery Disease
Your coronary arteries are like pipelines that deliver oxygen-rich blood to your heart muscle. Over time, lifestyle factors, genetics, and certain health conditions can cause plaque to accumulate along their walls. As plaque builds up, arteries narrow, reducing blood flow to the heart.
If the blood supply becomes too restricted, it can lead to:
- Angina (chest pain or discomfort during exertion)
- Shortness of breath
- Heart attack (if the artery becomes completely blocked)
Key Symptoms of Coronary Artery Disease
CAD can be a silent threat, with no symptoms in its early stages. When symptoms do appear, they may include:
- Chest discomfort or pain (angina), especially during physical activity
- Shortness of breath
- Pain radiating to the arm, neck, jaw, or back
- Unusual fatigue
- Nausea or lightheadedness
Importantly, symptoms can differ between individuals. Women, for example, are more likely to experience fatigue, nausea, and shortness of breath rather than classic chest pain.
Risk Factors You Can’t Ignore
The likelihood of developing CAD increases if you have:
- High LDL cholesterol or low HDL cholesterol
- High blood pressure
- Diabetes or insulin resistance
- Smoking history
- Sedentary lifestyle
- Family history of heart disease
- Obesity or metabolic syndrome
- Chronic stress or poor sleep
Why Early Detection Matters
By the time CAD causes noticeable symptoms, arterial narrowing may already have become significant. Early detection allows for lifestyle changes, medical treatment, and monitoring that can slow or even reverse disease progression.
Early diagnosis is also essential because CAD increases the risk of:
- Heart attack
- Heart failure
- Arrhythmias (abnormal heart rhythms)
- Sudden cardiac arrest
How Is CAD Diagnosed?
Doctors may use a combination of tests to identify CAD, including:
- Electrocardiogram (ECG) – Detects abnormal heart rhythms and signs of reduced blood flow.
- Echocardiogram – Uses ultrasound to visualize heart structure and function.
- Stress testing – Monitors heart performance during exercise.
- Coronary calcium scan – Measures calcium deposits in artery walls.
- Angiography – A detailed imaging test using contrast dye to map blood flow.
The Role of Long-Term ECG Monitoring in Early Detection
Traditional ECGs take a snapshot of your heart’s electrical activity in a few seconds. But coronary artery disease doesn’t always misbehave during a doctor’s visit – many abnormalities occur during daily activities, stress, or exercise.
That’s where long-term ECG monitoring shines.
Devices such as the FDA-cleared, chest strap-based, patchless Frontier X Plus provide high-fidelity ECG readings continuously, capturing subtle changes in heart rhythm or stress on the heart that short tests might miss.
Some of the ECG changes seen in CAD are ST segment depression, ST segment elevation, flattening of the T waves, inverted T waves
Importantly, if your heart experiences reduced blood supply during physical exertion, a continuous long-term ECG device may pick it up well before symptoms become obvious.
Treatment for Coronary Artery Disease
Once diagnosed, CAD can be managed with a combination of lifestyle changes, medications, and in some cases, procedures.
Lifestyle Changes
- Heart-healthy diet (low saturated fat, more fruits, vegetables, whole grains)
- Regular exercise (as recommended by your doctor)
- Smoking cessation
- Stress management
- Better sleep habits
Medications
Common CAD medications include:
- Statins – Lower cholesterol
- Beta-blockers – Reduce heart workload
- Antiplatelet agents – Prevent clot formation
- ACE inhibitors – Lower blood pressure and protect the heart
Procedures
- Angioplasty and stent placement – Opens blocked arteries
- Coronary artery bypass grafting (CABG) – Creates new routes for blood flow
Preventing CAD: A Lifelong Commitment
Even if you don’t currently have CAD, prevention is key:
- Know your risk factors and get regular checkups
- Maintain a healthy weight
- Stay active and avoid prolonged sitting
- Eat a balanced diet rich in omega-3 fatty acids
- Use wearable technology like Frontier X2 to track heart performance, especially if you have multiple risk factors or a family history of CAD
FAQs on Coronary Artery Disease
- What is the first sign of coronary artery disease?
Often, it’s chest discomfort during physical activity (angina), but some people experience fatigue, shortness of breath, or no symptoms at all in early stages. - Can CAD be reversed?
In some cases, aggressive lifestyle changes, medications, and risk factor management can slow, stop, or partially reverse plaque buildup. - How is CAD different from a heart attack?
CAD is the gradual narrowing of coronary arteries, while a heart attack occurs when one of these arteries becomes completely blocked. - Can continuous ECG monitoring detect CAD?
While it cannot diagnose CAD on its own, ECG devices that record continuously such as Frontier X2 can record detailed ECG data. This information can then be reviewed by a clinician, who may determine whether further testing for conditions such as ischemia or CAD is warranted. - What is the best treatment for CAD?
It depends on severity – mild cases may respond to lifestyle changes and medications, while advanced CAD might require angioplasty or bypass surgery.
Long-distance running and high-intensity training bring undeniable benefits for heart health, endurance, and overall fitness. However, the repetitive impact on your muscles, bones, and joints can lead to overuse injuries if your body isn’t given time to adapt. One emerging metric that athletes and sports scientists are paying closer attention to is body shock – the force your body experiences with every stride.
By tracking body shock in real time, athletes can better understand the mechanical stress their bodies are enduring and adjust their training to prevent injuries before they happen. In this article, we’ll explore what body shock is, why it matters, how to measure it, and how it can be used to safeguard your running performance.
What Is Body Shock?
Body shock refers to the physiological stress experienced by the body during intense physical exertion or when adapting to new fitness routines. More specifically, it refers to the vertical and horizontal impact forces transmitted through your body during foot strike when running. Each time your foot hits the ground, the energy of the impact travels from your foot up through your leg, hips, and spine. These shockwaves can influence both performance and injury risk.
The magnitude of body shock depends on several factors:
- Running surface (concrete, track, grass, treadmill)
- Footwear cushioning and fit
- Running technique (heel strike vs midfoot strike)
- Speed and stride length
- Fatigue level and muscle activation
When body shock is consistently high over time, it can cause microtrauma in muscles, tendons, and joints – setting the stage for injuries like shin splints, stress fractures, IT band syndrome, and lower back pain.
Why Tracking Body Shock Matters for Runners
1. Early Injury Prevention
Most running injuries start small – a bit of soreness in the shins, a dull ache in the hip. These early signs often go unnoticed or ignored until the pain is severe enough to interrupt training. By tracking body shock, runners can see when their impact loads are spiking, even before pain appears.
2. Optimizing Training Load
In endurance sports, the principle of progressive overload is key – you increase training stress gradually so your body can adapt. Tracking body shock helps ensure that your loading is progressive and not excessive, preventing sudden overload that the body isn’t ready for.
3. Technique Improvement
Poor form, overstriding, or landing with a stiff leg can increase shock loads. Real-time body shock data lets you experiment with changes – such as shortening your stride, increasing cadence, or improving core stability – and immediately see if those changes reduce impact.
4. Surface and Footwear Insights
Runners often switch between surfaces and shoes without realizing the changes in body shock they create. Measuring impact allows you to see whether your new trainers are actually reducing forces, or if running on trails is truly easier on your joints compared to the road.
How Body Shock Is Measured
Traditionally, measuring body shock required force plates in biomechanics labs – not practical for everyday runners. Today, wearable technology has changed that. Advanced continuous ECG and activity monitors can incorporate accelerometers and gyroscopes to track real-time impact forces during runs.
These devices can:
- Detect vertical impact force per step
- Show cumulative shock over the entire session
- Highlight shock spikes linked to fatigue or poor form
- Sync with training logs for trend analysis
When paired with heart rate and breathing data, body shock tracking becomes even more powerful, showing not just how much stress your body is experiencing, but also how your cardiovascular system is coping with it.
Common Injuries Linked to High Body Shock
- Shin Splints (Medial Tibial Stress Syndrome)
High impact forces can irritate the muscles and bone tissue around the tibia, leading to persistent shin pain. - Stress Fractures
Excessive loading without enough recovery time can cause microscopic cracks in bones, often in the tibia, metatarsals, or femur. - Runner’s Knee (Patellofemoral Pain Syndrome)
Repeated shock can aggravate the cartilage under the kneecap, especially in runners with poor tracking of the knee joint. - IT Band Syndrome
High side-to-side impact forces can cause inflammation in the iliotibial band, leading to sharp pain on the outer knee. - Lower Back Pain
Vertical shock forces travel through the spine, and poor shock absorption can contribute to back discomfort or injury.
Using Body Shock Data to Prevent Injuries
1. Adjusting Stride and Cadence
If your device shows consistently high impact, try shortening your stride and increasing your cadence (steps per minute). This spreads the load more evenly across muscles and reduces vertical oscillation.
2. Monitoring Fatigue
Fatigue often changes your running mechanics – you might land harder, lose form, and increase body shock. Tracking trends across a run helps you see where form breaks down so you can schedule rest days or strength work.
3. Choosing Recovery-Friendly Days
If body shock data shows unusually high values in one session, follow it with a low-impact workout – cycling, swimming, or walking – to allow tissues to recover.
4. Testing Footwear and Surfaces
Log body shock levels for different shoes and surfaces. Use this information to rotate shoes wisely and choose surfaces that keep your impact in a safe range.
5. Strength and Stability Work
Reducing body shock isn’t just about softer landings – stronger muscles and better stability help absorb and control forces. Strengthening the calves, quads, hips, and core can lower shock over time.
The Future of Running Injury Prevention
The combination of wearable technology and data-driven training is changing how athletes manage injury risk. Instead of reacting to pain after it appears, runners can now see stress patterns in real time and make immediate changes.
Body shock tracking is likely to become a standard metric in sports performance, much like heart rate monitoring. As more runners embrace this technology, training programs will shift from one-size-fits-all mileage targets to personalized load management plans that protect long-term health.
The Frontier X2 Advantage: Integrating Body Shock with Long-Term ECG Monitoring
Modern runners are no longer limited to just tracking pace and distance. Devices like Frontier X2 combine long-term-ECG monitoring with motion-sensing technology, giving athletes real-time insight into both mechanical and cardiac stress.
This integration is game-changing: while body shock data shows how much impact your body absorbs, ECG tracking reveals how your heart responds to that load. For instance, runners can correlate increased heart rate or arrhythmic patterns with moments of elevated shock, highlighting fatigue or stress points that require attention.
By uniting cardiac and biomechanical analytics, Frontier X2 empowers runners to train smarter, optimize recovery, and reduce injury risks – ensuring performance safety from both a musculoskeletal and cardiovascular standpoint.
Understanding Impact Loading Rate for Safer Running
Tracking body shock, measured as impact loading rate (in bodyweight per second or BW/s), provides valuable insights for injury prevention. Typical loading rates range from 45–65 BW/s:
- <45 BW/s: Softer landings, often seen in midfoot strikers or cushioned shoes
- >65 BW/s: Rapid force application, higher injury risk, common in heel strikers
While ECG changes during exercise don’t directly affect loading rate, they reflect cardiovascular effort, which can indirectly influence running mechanics and shock absorption. Using this data, runners can fine-tune gait, cadence, and training load to minimize harmful impact forces.
Key Takeaways
- Body shock measures the impact forces your body experiences during running.
- Consistently high body shock can lead to overuse injuries like shin splints, stress fractures, and knee pain.
- Tracking body shock in real time allows you to adjust form, manage fatigue, and prevent injuries before symptoms appear.
- Wearable tech now makes body shock measurement accessible for everyday runners, not just lab studies.
- Combining body shock data with heart rate, cadence, and training load creates a complete picture of your running health.
FAQs
Q1: What is body shock when running?
Body shock refers to the impact forces traveling through your body when your foot strikes the ground during running.
Q2: How does high body shock cause injuries?
High impact over time can stress bones, muscles, and joints, leading to overuse injuries like shin splints or stress fractures.
Q3: Can footwear reduce body shock?
Yes. Well-cushioned, properly fitted shoes can reduce impact, but technique and training load also matter.
Q4: How can I measure body shock at home?
Modern wearable devices with motion sensors can track body shock during training and display it on connected apps.
Q5: Does running on softer surfaces lower body shock?
Often yes – grass or trails generally produce lower forces than concrete, but technique still plays a big role.
Your heart is an incredibly responsive organ, adapting beat by beat to your emotions, activity level, and physiological needs. But what happens when it skips a beat or adds an extra one? While it might feel alarming, not all irregular heartbeats are cause for panic. Two of the most common culprits behind these extra beats are Premature Atrial Contractions (PACs) and Premature Ventricular Contractions (PVCs). Though often benign, understanding the difference between them is essential for anyone looking to monitor and manage their cardiovascular health.
In this blog, we’ll break down what PACs and PVCs are, how they differ, what causes them, and how continuous ECG monitoring can help detect, interpret, and manage these irregular rhythms.
Understanding the Basics: What Are PACs and PVCs?
Premature Atrial Contractions (PACs) are early heartbeats that originate in the atria, the upper chambers of the heart. Essentially, an extra electrical signal fires before the normal heartbeat is due, causing the atria to contract prematurely.
Premature Ventricular Contractions (PVCs), on the other hand, are extra beats that originate in the ventricles, the lower chambers of the heart. They occur when an ectopic focus in the ventricle sends out an impulse too early, disrupting the regular heartbeat.
While both PACs and PVCs are classified as types of ectopic (or out-of-place) beats, the location of their origin defines their impact and potential significance.
What Do They Feel Like?
Both PACs and PVCs can feel like:
- A skipped beat
- A fluttering sensation
- A brief pounding in the chest
- A pause followed by a stronger heartbeat (due to the compensatory pause)
However, many people don’t feel them at all. These irregularities are often discovered incidentally during routine ECGs or while wearing a heart monitor.
How Are They Different?
- Point of Origin
- PACs originate in the atria.
- PVCs originate in the ventricles.
- ECG Characteristics
- PACs appear as early P waves with abnormal shapes, often followed by a normal QRS complex.
- PVCs present as wide and bizarre-looking QRS complexes not preceded by P waves.
- Clinical Implication
- PACs are often benign and may not require treatment.
- PVCs, particularly when frequent or in patterns like couplets or triplets, may require further evaluation as they could signal underlying heart disease.
Common Causes
Shared Causes:
- Stress or anxiety
- Caffeine, alcohol, or stimulant use
- Electrolyte imbalances
- Fatigue or lack of sleep
- Fever or dehydration
Specific to PACs:
- Hyperthyroidism
- Lung disease (e.g., COPD)
Specific to PVCs:
- Structural heart disease
- Post-heart attack scar tissue
- Cardiomyopathy
Are They Dangerous?
In healthy individuals, occasional PACs and PVCs are usually harmless. However, their context matters:
- Isolated PACs are rarely dangerous and often resolve on their own.
- Frequent PACs may increase the risk of developing atrial fibrillation (AFib).
- Isolated PVCs are often benign, especially in younger people.
- Frequent PVCs (more than 10,000 per day) may be linked to a higher risk of cardiomyopathy or sudden cardiac events, particularly if accompanied by symptoms like dizziness or shortness of breath.
When Should You Be Concerned?
If you experience any of the following, it’s time to seek medical attention:
- Palpitations that persist or worsen
- Lightheadedness or fainting
- Chest pain or discomfort
- Shortness of breath
- Irregular heartbeat during exertion
These symptoms could point to underlying cardiac issues, and further diagnostic workup including echocardiogram, stress testing, or longer-term ECG monitoring may be necessary.
The Role of Continuous ECG Monitoring
Standard in-clinic ECGs or even short-duration Holter monitors may miss intermittent PACs and PVCs. This is where continuous ECG monitoring makes a difference. These wearable monitors allow for:
- 24/7 real-time ECG capture of arrhythmic events
- Event tagging, so users can record symptoms like palpitations or dizziness
- Long-duration use, increasing the chances of detecting infrequent ectopic beats
- Detailed rhythm analysis, distinguishing between PACs, PVCs, and other arrhythmias
By tracking heart rhythms across sleep, activity, and stress states, continuous monitors help paint a more accurate picture of your cardiac health.
How Continuous ECG Monitoring Helps Different Populations
- Athletes: Who often report skipped beats post-training. Continuous monitoring can help differentiate benign PACs/PVCs from more concerning arrhythmias.
- Post-COVID patients: Some individuals report new-onset palpitations or ectopic beats during recovery. Monitors can assist in determining if these are PACs, PVCs, or signs of myocarditis.
- Older adults: As age increases, so does the prevalence of ectopic beats. Monitoring ensures early detection of progression to more serious arrhythmias like AFib.
- Patients with known heart disease: Continuous data allows clinicians to assess risk, medication effectiveness, and potential need for electrophysiological intervention.
Interpreting the Results
Only a qualified medical professional can determine whether your ectopic beats are harmless or a warning sign. After your continuous ECG data is reviewed, your doctor might suggest:
- Lifestyle adjustments (reducing caffeine, stress, or alcohol)
- Medication to suppress ectopic beats if symptomatic
- Further testing, such as echocardiograms or stress tests
- Electrophysiology referral, if the burden of PVCs or the complexity of PACs is high
- Good Sleep
Final Thoughts
While PACs and PVCs can be unsettling, they are extremely common and often benign. The key to managing them is context: understanding when they occur, how frequently, and whether they are accompanied by symptoms or structural heart abnormalities.
Continuous ECG monitoring provides the long-term, detailed data needed to demystify these extra beats and ensure they don’t go undetected or misunderstood. With the right tools and guidance, individuals can take charge of their heart health with clarity and confidence.
If you’ve ever felt your heart skip a beat or flutter unexpectedly, know that answers are within reach. Speak to your healthcare provider about whether continuous ECG monitoring could help uncover what your heart is really telling you.
A fast heartbeat during a workout is expected – after all, your heart is working harder to meet your body’s increased oxygen demands. But what if your rapid heart rate isn’t normal? How do you distinguish between exercise-induced tachycardia and arrhythmic tachycardia, which could signal a deeper cardiac issue?
Understanding the difference can be tricky, even for clinicians. In this blog, we break down the challenge of detecting tachycardia caused by exertion versus that triggered by a heart arrhythmia, and how long-term ECG monitors can help reveal the truth behind your elevated heart rate.
What Is Tachycardia?
Tachycardia is defined as a heart rate exceeding 100 beats per minute (bpm) at rest. It’s important to remember that not all tachycardia is abnormal. For instance:
- Exercise-induced tachycardia is a healthy physiological response to physical exertion.
- Arrhythmic tachycardia (such as ventricular tachycardia, SVT arrhythmia, or atrial tachycardia) stems from abnormal electrical signaling and can be dangerous, especially if persistent or occurring at rest.
Why the Confusion?
During exercise, it’s normal for your cardiac rhythms to increase – sometimes even hitting 160–180 bpm depending on your age and fitness level. However, symptoms like:
- Lightheadedness
- Sudden fatigue
- Fluttering or pounding sensation in the chest
- Shortness of breath beyond your fitness norm
…may signal something more serious, such as atrial fibrillation (AF), atrial flutter, or even ventricular tachycardia.
Some people experience paroxysmal arrhythmias – episodes that come and go unpredictably, making them hard to catch during routine ECGs or annual checkups. That’s where continuous, activity-aware monitoring becomes essential.
Comparing the Two: At a Glance
| Feature | Exercise-Induced Tachycardia | Arrhythmic Tachycardia |
| Triggered by | Physical exertion | Abnormal electrical impulses in the heart |
| Heart Rate Behavior | Gradual rise/fall with activity | Sudden onset and often irregular |
| Symptoms | Usually asymptomatic | Dizziness, palpitations, chest pain |
| Rhythm | Regular sinus rhythm | May be irregular (e.g., AF ECG) |
| Resolution | Resolves post-exercise | May persist or worsen without treatment |
The Diagnostic Gap
Most traditional diagnostics, like resting ECGs or Holter monitors, offer only a short snapshot of your heart’s activity. And smartwatches, while popular, often rely on brief 30-second recordings that may not capture EKG arrhythmia events occurring during high motion.
This diagnostic gap can lead to missed abnormal heart rhythms, delayed care, and ongoing uncertainty for patients who feel “something’s off” during workouts.
How Can Long-term ECG Monitors Help Clarify Heart Rhythm During Exercise?
If you’re experiencing a rapid heartbeat during exercise, it can be difficult to know whether it’s simply your heart responding to physical effort or something more irregular. Long-term ECG monitors can provide clinicians with detailed, high-fidelity ECG data that helps them interpret how your heart behaves under physical stress.
Unlike smartwatches or brief, spot-check devices, these chest-worn monitors record high-quality ECG waveforms for hours at a time, including during intense activity and recovery. This continuous data stream gives your physician the full picture – not just your heart rate, but the rhythm patterns that go with it.
Here’s how long ECG monitors assist in understanding exercise-related tachycardia:
- Detailed ECG Waveform Capture: These devices collect full ECG strips during your entire workout and rest phases. This allows physicians to assess if your rhythm follows a normal, progressive sinus pattern, or if irregularities like atrial flutter, SVT, or other abnormal beats are present.
- Symptom and Activity Tagging: Through the companion app, users can mark when they’re exercising or experiencing symptoms. This context helps physicians correlate your rhythm strips with specific events like warm-up, peak exertion, or cool-down.
- Detection of Intermittent Rhythm Irregularities: Paroxysmal arrhythmias often occur unpredictably. Because Frontier X Plus record ECG continuously, they can capture fleeting rhythm disturbances that might otherwise go unnoticed in clinic-based ECGs or 30-second smartwatch checks.
- Post-Exercise Monitoring: Some irregular heart rhythms show up after exercise ends, during recovery, when autonomic shifts occur. These prescription devices track your heart rhythm throughout this transition, helping your doctor observe how your heart resets itself.
- Remote Access and Graph Review: The data is securely synced to a cloud-based platform, allowing clinicians to log in and review time-stamped ECG strips in detail. This enables them to assess heart rhythm patterns over time and provide guidance based on concrete, objective trends, not just reported symptoms.
In short, long-term ECG monitors support a more informed understanding of how your heart functions during physical activity, helping your healthcare provider make timely, evidence-backed decisions about your next steps.
Who Should Monitor Their Heart During Workouts?
- Endurance athletes and fitness enthusiasts
- Anyone who experiences unexplained fatigue or dizziness while exercising
- Individuals with a family history of cardiovascular arrhythmia
- People recovering from a heart procedure or with diagnosed AF, or ventricular tachycardia
Final Thoughts
It’s easy to assume that a fast heart rate during exercise is normal, and often it is. But when it isn’t, you deserve more than guesswork. Understanding whether your rapid heartbeat is a healthy response or a warning sign requires more than a stopwatch or a wrist tap.
With ECG monitors that record continuously, you and your doctor can finally decode your heart’s signals and distinguish between fitness and concern.
Don’t let uncertainty stop you from reaching your goals. Trust your instincts, monitor your rhythms, and move forward with clarity.
Your heart is more than a symbol of emotion – it’s a finely tuned muscle responsible for pumping blood throughout your body with precision. A normal resting heart rate for adults typically falls between 60 to 100 beats per minute (bpm). But what happens when your heart beats too fast or too slow? That’s where conditions like tachycardia and bradycardia come in.
In this blog, you’ll explore what these terms mean, what your heart rate might be telling you, and how ECG monitoring tools can help detect silent or intermittent heart rhythm issues before they become serious.
When Slower Isn’t Always Better
Take Olympic swimmer Mark Spitz, for example. Known for his elite athleticism, Spitz was diagnosed with bradycardia in 2018. Despite being in peak physical shape, he experienced symptoms after intense training sessions. What seemed like fatigue turned out to be a dangerously low heart rate. With early detection and proper monitoring, he was able to adjust his routine and manage his condition, proving that even champions aren’t immune to heart arrhythmias.
Spitz’s experience is a powerful reminder that a slow heart rate isn’t always a sign of fitness – sometimes, it’s a sign to pay attention. With the right tools and awareness, even hidden rhythm issues can be uncovered and managed before they become serious.
What Is Bradycardia?
Bradycardia is the opposite – a slower-than-normal resting heart rate, typically under 60 bpm. For some people, especially athletes, a slow heart rate can be a sign of strong cardiovascular health. But if your heart is beating too slowly to supply enough oxygen-rich blood to your body, it may result in:
- Fatigue
- Dizziness or lightheadedness
- Shortness of breath
- Fainting (syncope)
Bradycardia can be caused by issues in the heart’s natural pacemaker (the SA node), medication side effects, or underlying heart disease. Just like with tachycardia, not all cases are symptomatic, making it essential to track heart rhythms over time.
What Is Tachycardia?
Tachycardia refers to a resting heart rate that’s higher than normal, generally over 100 bpm in adults. It’s like your heart is revving its engine even when you’re parked. While it can be a normal response to exercise, stress, or excitement, persistent or unexplained tachycardia can signal an underlying issue.
There are several types of tachycardia:
- Ventricular tachycardia (VT): Starts in the lower chambers and can be life-threatening if not treated.
- Supraventricular tachycardia (SVT): A fast heart rate that begins above the ventricles, in the atria.
Some people feel symptoms like palpitations, chest discomfort, or shortness of breath. Others may not notice anything at all, which is why monitoring is so important.
Quick Guide: Heart Rate Ranges & What They Might Mean
| Heart Rate (bpm) | Classification | Possible Implications |
| Below 60 | Bradycardia | May be normal in athletes; could signal SA node dysfunction if symptomatic |
| 60–100 | Normal | Healthy resting heart rate for most adults |
| 100–130 | Mild Tachycardia | Could result from stress, fever, dehydration, physical activity or stimulant use |
| 130–160+ | Severe Tachycardia | Could result from intense exercise. May also indicate arrhythmia like SVT or VT- medical evaluation recommended |
Note: Heart rate should always be interpreted in the context of age, activity level, and symptoms.
Why Does Heart Rate Matter?
Your heart rate is a window into your cardiovascular health. While momentary fluctuations are normal, consistently high or low rates can lead to complications if left unchecked, including:
- Blood clots
- Heart failure
- Stroke
- Sudden cardiac arrest
What makes both tachycardia and bradycardia tricky is their potential to appear intermittently, especially during sleep, rest, or physical activity. These episodes may be missed by standard in-clinic ECGs or short-term Holter monitors.
Tachycardia and Bradycardia in Context: Beyond Resting Heart Rate
It’s important to note that both tachycardia and bradycardia aren’t limited to resting heart rate patterns alone. These rhythms can fluctuate during sleep, stress, hydration changes, or while transitioning between rest and exertion. For instance, inappropriate sinus tachycardia – where the heart races without clear triggers – and paroxysmal bradycardia – brief drops in heart rate that may cause fainting – are both challenging to catch with standard checkups. ECG monitoring bridges this gap by capturing these rhythm changes dynamically, offering clinicians more complete diagnostic insight into when and why these fluctuations occur.
When the Heart Swings: Alternating Bradycardia and Tachycardia
Some individuals may experience a condition known as tachy-brady syndrome, where the heart alternates unpredictably between too-slow and too-fast rhythms. This is particularly common in patients with sick sinus syndrome, a dysfunction of the heart’s natural pacemaker. These erratic swings can go unnoticed for years, especially if symptoms are mild or sporadic – such as occasional fatigue, brain fog, or palpitations. However, the consequences can be serious, including syncope or even sudden cardiac arrest. ECG monitoring is vital in capturing these transitions and enabling timely interventions, such as medication adjustments or pacemaker implantation if needed.
How ECG Monitoring Helps
This is where patchless ECG monitors come into play. Worn comfortably on the chest, it records high-quality ECG data in near-real-time, whether you’re working, resting, or exercising.
With the ECG monitors, you can:
- Capture both sinus rhythm and abnormal heart patterns like arrhythmia, SVT, or ventricular tachycardia.
- Tag symptoms during episodes for better physician interpretation.
- Sync data via a companion app for remote clinician access.
- Receive end-of-study reports reviewed by cardiac physiologists or your care team.
Unlike smartwatches that rely on 30–60 second spot checks, ECG monitors continuously record data for up to 24 hours per charge – making it much more effective at identifying silent or intermittent arrhythmias.
Who Should Be Monitoring Their Heart Rate?
You don’t have to wait for symptoms to take control of your heart health. ECG monitoring is especially helpful for:
- Individuals with known or suspected atrial fibrillation (AF)
- Those experiencing fluttering in the heart or palpitations
- Patients recovering from cardiac procedures
- Athletes pushing through endurance training
- Anyone with a family history of cardiovascular arrhythmia or abnormal heart rhythm
When to Talk to Your Doctor
If you’ve experienced:
- Skipped or irregular beats
- Rapid heart rate without exertion
- Lightheadedness or fatigue
- Nighttime chest discomfort or palpitations
It’s time to speak with your doctor. They may recommend a clinical-grade EKG/ECG machine or wearable electrocardiogram monitors for home use.
Final Thoughts
Your heart rate isn’t just a number – it’s a message from your body. Conditions like tachycardia and bradycardia might seem mild or go unnoticed at first, but over time, they can lead to serious outcomes. The good news? With advancements in ECG monitor technology, you can catch these issues early and take action.
Whether you’re trying to understand an odd flutter in your chest, monitor your atrial fibrillation heart rate, or manage a known condition, tools like ECG monitors provide clarity and control. They bridge the gap between how you feel and what your heart is actually doing – 24/7.
Don’t wait for a scary symptom to listen to your heart. Start monitoring today, and give your heart the attention it deserves.
Even the Fittest Can Miss the Signs
Atrial fibrillation doesn’t discriminate – it affects everyone from retired teachers to celebrities and world-class athletes. Basketball legend Larry Bird continued competing through dizzy spells later identified as AFib. Olympic swimmer Mark Spitz, despite his elite fitness, was blindsided by the diagnosis after a post-workout episode. Even public figures like former US presidents Joe Biden and George HW Bush, Arnold Schwarzenegger, and Susan Lucci have spoken openly about living with atrial fibrillation. What connects them all isn’t just their status — it’s the fact that AF often creeps in silently, revealing itself only through persistent monitoring. Their stories underscore an important truth: staying fit doesn’t mean you’re immune to cardiac arrhythmias, and that’s exactly why continuous ECG/EKG monitors are important for uncovering what you can’t always feel.
These stories underscore a powerful truth: staying fit doesn’t mean you’re immune to cardiac arrhythmias. Continuous ECG/EKG monitors are critical for uncovering what you can’t always feel.
If you’re someone who pushes hard during a run, a bike ride, or even a dance class — and feel the occasional flutter, breathlessness, or moment of fatigue — don’t ignore it. You might feel strong, but your heart could be telling a different story. That’s where the continuous EKG monitoring technology gives you power: real insight when you need it most.
Why Exercise Can Trigger or Reveal Arrhythmias
Exercise can trigger arrhythmias by placing acute stress on the heart’s electrical system through increased sympathetic activity, elevated heart rate, and electrolyte imbalances from sweating. In individuals with genetic predispositions or structural heart conditions, this stress may provoke arrhythmias such as atrial flutter, supraventricular tachycardia (SVT), or even ventricular tachycardia
Additionally, sudden vagal rebound after intense workouts may destabilize the heart rhythm, particularly in endurance athletes. While exercise is beneficial for most, these physiological changes can unmask hidden electrical instability, making continuous ECG monitoring during and after exercise a critical tool for early detection.
Research indicates that overtraining or prolonged high-intensity activity may lead to atrial remodeling and increase the risk of AF over time — especially in athletes who have participated in endurance sports for many years. Thus, identifying early signs through wearable tech can prevent more serious episodes.
Symptoms to Watch During or After Exercise
If you have an underlying arrhythmia, symptoms may appear only when your heart is under pressure. These include:
- Shortness of breath
- Unexplained fatigue
- Rapid, irregular, or pounding heartbeat
- Dizziness or lightheadedness
- Chest discomfort or palpitations
Some people feel just a flutter; others may feel nothing at all. These subtle signs could point to atrial fibrillation or other heart irregularities that require evaluation
Unfortunately, Around one-third of those with AFib may not experience symptoms. — highlighting the importance of vigilance.
Who’s at Risk for Exercise-Triggered Arrhythmias?
- Aged adults — especially those with hypertension or prior history of cardiovascular arrhythmia
- Endurance athletes with long training histories (marathoners, triathletes, cyclists)
- Individuals with diagnosed Atrial Fibrillation (AF) with rapid ventricular response
- People with a family history of AFib or inherited arrhythmia syndromes
- Those experiencing increased palpitations, chest pressure, or breathing difficulty post-exercise
Long-term endurance sport practice is linked to a higher incidence of lone AF in men.
The Role of Continuous ECG Monitoring in Fitness
Traditional 12-lead ECG tests or short-term Holter monitors rarely capture arrhythmias that occur during physical exertion or recovery. That’s where continuous ECG monitoring becomes essential for active individuals.
These monitors offer:
- Continuous detection of AF events, bradycardia, and tachycardia
- Symptom tagging during workouts for contextual insight
- Instant syncing of ECG data to the app upon device connection, enabling timely clinician review.
Unlike smartwatches that offer brief 30-second spot checks, ECG monitors like the FDA-cleared, prescription-based Frontier X Plus and wellness-based Frontier X2 provide continuous, high-fidelity ECG data. This allows physicians to overread the recordings and detect arrhythmias that may occur during physical exertion – events often missed by short-duration monitors..
Key features include:
- Patchless and sweat-resistant, making it ideal for prolonged use during physical activity
- Delivers high-fidelity ECG data continuously, even during intense workouts
- Provides clinically reviewed summaries post-monitoring (especially if you have been prescribed a Holter monitor)
- Beneficial for individuals with existing heart conditions, athletes in post-treatment recovery, or anyone experiencing unexplained symptoms during exertion
Continuous ECG monitoring helps:
- Enable early detect for silent AF episodes
- Empower users to manage their heart health proactively
Empowering the Fitness-Minded With Better Tools
Whether you’re training for a race or simply trying to stay fit, ECG monitoring should not be an afterthought. Continuous ECG/EKG devices provide an unprecedented view into your cardiovascular rhythms — delivering actionable insights that you and your doctor can use to guide your care.
Athletes who report fluttering, skipped beats, or fatigue but receive “normal” clinic ECGs may simply not be monitored at the right time — typically when they’re resting. This is precisely why capturing data during and immediately after exertion is essential.
Moreover, for patients recovering from procedures like ablation or managing chronic AF through medication, these devices serve as a personalized health companion. They make it easier to recognize if interventions are working or if further changes are needed.
Final Thoughts
Exercise-induced arrhythmias are more common than you may think — and they often go unnoticed without the right monitoring. Whether you’re managing AF, atrial flutter, VT, SVT, or any form of EKG-detected arrhythmia, being proactive is key.
Wearable ECG monitors help bridge the gap between exercise and detection, allowing active individuals to train smarter, protect their long-term cardiovascular health, and gain peace of mind.
If you’ve experienced any irregular symptoms during workouts, or want to monitor your heart rhythm more closely, speak to your physician about using a continuous ECG/EKG device.
When it comes to heart health, there’s one truth many people don’t realize until they experience it firsthand: the rhythm of your life often mirrors the rhythm of your heart.
If you’ve been diagnosed with atrial fibrillation (AFib) – the most common atrial arrhythmia – you know how unsettling it can be. AFib causes the upper chambers of your heart (the atria) to quiver chaotically instead of beating in a steady, sinus rhythm. This leads to an irregular and often rapid heart rate, creating sensations like palpitations, a pounding heartbeat, dizziness, or even chest discomfort.
While medications and procedures like ablation play a critical role in treatment, many people overlook a key part of managing AFib: understanding and controlling personal lifestyle triggers.
In this blog, we’ll break down how daily habits – especially alcohol, caffeine, stress, and sleep patterns – may be silently influencing your heart rhythm. We’ll also explain how long-term ECG monitoring can help you identify your unique AFib patterns and make more informed choices to protect your heart health.
Why Triggers Matter in AFib Management
AFib isn’t always constant. For many people, it’s paroxysmal, meaning episodes come and go. The tricky part is that the triggers aren’t the same for everyone. Some people might notice their AFib symptoms right after a glass of wine, while others experience irregular beats following a stressful day or poor sleep.
The more you understand what sets off your episodes, the more control you can regain over your daily life. By identifying triggers early, you can:
- Reduce AFib burden (how often you experience episodes)
- Avoid progression to persistent or paroxysmal AFib
- Lower the risk of stroke, heart failure, and other complications
- Improve quality of life by reducing palpitations and discomfort
Alcohol and AFib: What the Research Shows
Does drinking alcohol increase heart rate?
In short: yes – for many people, it does.
Alcohol is one of the most well-documented AFib triggers. Studies show that even small amounts of alcohol can raise the risk of an AFib episode. In fact, the term “Holiday Heart Syndrome” was coined decades ago after doctors noticed a spike in arrhythmias during holiday seasons when people tend to drink more.
How Alcohol Affects Heart Rhythm
- Alcohol alters electrical signals in the atria, making it easier for chaotic rhythms to develop.
- It can cause dehydration, which throws off your body’s electrolyte balance – critical for a normal heartbeat.
- Alcohol may increase blood pressure, compounding the strain on your heart.
- Over time, heavy drinking can lead to cardiomyopathy, weakening the heart muscle itself.
What About Moderate Drinking?
Even moderate consumption – such as one drink a day – can raise your AFib risk. A meta-analysis published in Frontier of Cardiovascular Medicine found that a 1 drink/day increase in alcohol consumption increased the risk of AF by 6%
If you have AFib, doctors generally recommend limiting or avoiding alcohol. But the best way to know how it affects you personally is by tracking your episodes in real time.
Caffeine and AFib: Friend or Foe?
Coffee and high blood pressure have long been associated, but what about caffeine and AFib?
This is where things get a little more complicated. For years, doctors advised patients with atrial arrhythmia to avoid caffeine entirely. However, recent research suggests the link may not be as straightforward.
What the Studies Say
- Some people are sensitive to caffeine, and even a small amount can cause palpitations or an erratic heart rhythm.
- For others, moderate coffee intake may actually be neutral or even protective for the heart.
- Energy drinks, however, often contain very high levels of caffeine combined with other stimulants and have been linked to dangerous ventricular activity and arrhythmias.
Bottom Line on Caffeine
If you’ve noticed that your heart feels like it is racing after coffee or tea, it’s worth experimenting by cutting back. Keep in mind that continuous heartmonitoring can help determine whether your ventricular rhythm types or atrial rhythm patterns are actually changing after caffeine intake.
Stress and Sleep: The Silent Contributors
Stress and atrial fibrillation are closely linked. Emotional stress triggers a surge of catecholamines – hormones that speed up your heart rate and can tip your system into AFib.
Poor sleep is another hidden culprit. Conditions like sleep apnea or insomnia increase your risk of AFib by contributing to heart strain, spikes in blood pressure, and changes in heart rhythm during the night.
How to Track the Impact
- Keep a symptom journal noting stressful events, restless nights, or panic episodes.
- Use wearable ECG monitors that track your heart rate during sleep and heart rhythm at rest to identify nighttime disturbances.
How Long-TermECG Monitoring Helps You Stay Ahead
Standard checkups or Holter exams only offer a snapshot of your heart’s activity. But atrial fibrillation could often happen outside the doctor’s office.
That’s why long-termECG monitoring devices are becoming an essential part of AFib management. These wearable devices:
- Record both sinus rhythm and arrhythmias over 24 hours or longer
- Help correlate symptoms like palpitations with real ECG data
- Allow you to see how specific activities (like drinking alcohol or exercising) affect your heart rhythm
- Provide detailed reports for your healthcare provider to adjust treatment
Unlike basic fitness trackers, ECG monitors that record continuously, such as the Frontier X Plus, provide high-fidelity ECG and detect Afib episodes.
Practical Tips to Reduce Your AFib Triggers
Managing AFib isn’t just about medications or heart failure treatment – it’s also about lifestyle. Here’s how you can reduce your episodes:
- Limit or avoid alcohol, especially binge drinking.
- Monitor your caffeine intake. May try decaf or reduce portion sizes if you’re sensitive.
- Prioritize good sleep hygiene. Treat sleep apnea if diagnosed.
- Manage stress with relaxation techniques like yoga, meditation, or breathing exercises.
- Track your episodes with a heart rhythm monitor to spot personal patterns.
- Discuss findings with your doctor to adjust your AFib treatment plan.
Final Thoughts
Understanding your personal AFib triggers – whether it’s drinking and atrial fibrillation, caffeine and AFib, or emotional stress – empowers you to live a fuller, healthier life. By pairing lifestyle awareness with tools like long-termECG monitoring, you can make informed decisions that help protect your heart health and reduce the burden of atrial fibrillation.
Whether you’re dealing with occasional palpitations or frequent arrhythmia episodes, tracking your heart rhythm daily gives you and your doctor the data needed to adjust care and reduce future risks.
FAQs
Can alcohol cause AFib to start suddenly?
Yes. For many people, even a single drink can trigger a sudden episode of atrial fibrillation, especially if they are already predisposed.
Does coffee increase AFib risk?
Caffeine sensitivity varies. Some people find that coffee causes palpitations, while others do not experience any effect on their heart rhythm.
How can I monitor my AFib triggers at home?
Using a long-termECG monitor allows you to track your heart rhythm throughout the day and correlate arrhythmia episodes with specific triggers like alcohol, caffeine, or stress.
What is the best treatment for AFib triggered by lifestyle factors?
In addition to AFib medications, lifestyle modifications such as reducing alcohol, managing stress, and improving sleep can significantly reduce episodes.
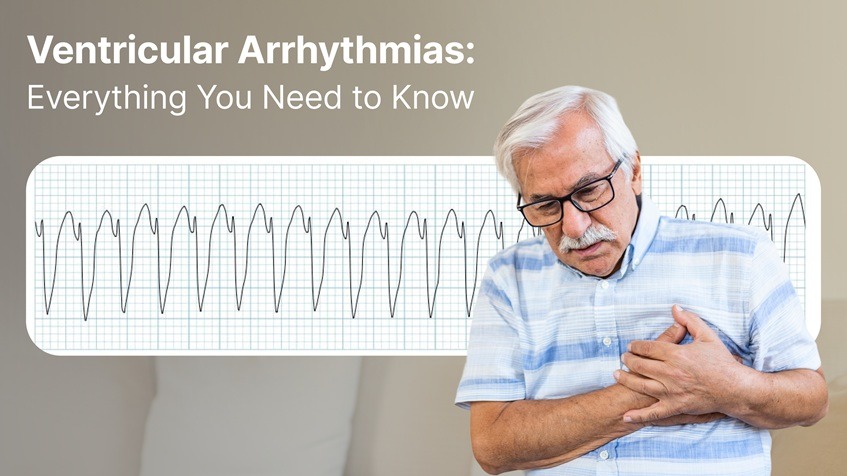
When your heart beats too fast, too slow, or erratically, it can feel like something is off. If you’ve ever thought, “My heart feels like it is racing,” or experienced a sudden, rapid heartbeat out of nowhere, you’re not alone. For many people, these sensations may be signs of ventricular arrhythmias, a group of heart rhythm disturbances originating in the lower chambers of the heart – the ventricles.
These conditions range from premature beats to potentially life-threatening rhythms like ventricular tachycardia (V Tach) and ventricular fibrillation (V Fib). Understanding these irregular rhythms is critical because early detection and management can prevent severe complications, including sudden cardiac arrest.
This comprehensive guide breaks down everything you need to know about ventricular arrhythmias, from their causes to treatment options and the latest in monitoring technology.
What Are Ventricular Arrhythmias?
Ventricular arrhythmias refer to abnormal electrical signals in the heart’s ventricles – the two lower chambers responsible for pumping blood to the lungs and the rest of the body. These disturbances can lead to inefficient blood flow, resulting in symptoms like dizziness, palpitations, fainting, or even cardiac arrest.
Types of Ventricular Arrhythmias
Understanding ventricular rhythm types is essential because not all ventricular arrhythmias are equally dangerous. Here’s a breakdown:
- Premature Ventricular Contractions (PVCs): They are early, extra heartbeats that start in the heart’s lower chambers (the ventricles), disrupting the heart’s normal rhythm for a moment
- Ventricular Tachycardia (V Tach): It is a rapid heart rhythm – more than 100 beats per minute – that begins in the lower chambers of the heart. This condition prevents the heart’s chambers from filling adequately with blood, reducing the amount that is pumped to the body.
- Ventricular Fibrillation (V Fib): is a life-threatening heart rhythm where the ventricles quiver or fibrillate chaotically instead of expanding and contracting effectively. This prevents the heart from pumping out blood. Within seconds, blood flow to the brain stops, causing loss of consciousness. Without immediate treatment, usually with defibrillation, V-Fib leads to sudden cardiac arrest.
Symptoms of Ventricular Arrhythmias
Many patients describe ventricular arrhythmias as feeling like a “sudden rapid heartbeat” or an erratic heart rhythm. Other common symptoms include:
- Chest pain or discomfort
- Dizziness or fainting (syncope)
- Shortness of breath
- Palpitations or fluttering sensations in the chest
- Fatigue or weakness
These symptoms often trigger a search for a heart monitor to check for arrhythmia, which helps confirm the diagnosis.
What Causes Ventricular Arrhythmias?
Several factors can lead to abnormal ventricular activity:
- Coronary artery disease
- Cardiomyopathy (weak or enlarged heart muscle)
- Heart failure
- Previous heart attack (myocardial infarction)
- Electrolyte imbalances
- Genetic conditions like arrhythmogenic right ventricular cardiomyopathy (ARVC)
- Medications or stimulant abuse
- Structural heart changes
In some cases, the cause remains unknown – a condition called idiopathic ventricular arrhythmia.
Why Are Ventricular Arrhythmias Dangerous?
Ventricular arrhythmias are a leading reason for cardiac arrest, especially when they progress to V Fib. The rapid and disorganized contractions prevent the heart from pumping blood, cutting off oxygen to the brain (cardiac arrest) and other vital organs. Without immediate intervention, this can lead to death within minutes.
Even if life-threatening events are avoided, heart rhythm problems like sustained V Tach can weaken the heart over time, increasing the risk of heart failure and other complications.
Diagnosing Ventricular Arrhythmias
If you suspect a ventricular rhythm issue, healthcare providers will often recommend a combination of tests:
Common Diagnostic Tools:
- Electrocardiogram (ECG):
The first-line test to detect arrhythmias in real-time. - Medical Holter Monitor:
A portable device worn for 24 to 48 hours to catch intermittent heart rhythm disturbances. - Event Monitors & Loop Recorders:
Long-term devices for patients with infrequent but concerning symptoms. - Echocardiogram & Cardiac MRI:
Used to check for structural abnormalities contributing to arrhythmias. - Electrophysiology Study (EPS):
A specialized test to map the heart’s electrical pathways and identify the source of abnormal signals. - Exercise stress test : if symptoms occur under exertion, exercise stress tests will often be ordered to look for these conditions
Treatment Options for Ventricular Arrhythmias
Treatment depends on the type and severity of the arrhythmia, symptoms, and underlying causes.
Medications
- Antiarrhythmic Drugs:
These are prescribed to stabilize ventricular activity. Common ventricular tachycardia treatment drugs include amiodarone and lidocaine. - Beta-Blockers:
Reduce the risk of dangerous arrhythmias, especially in patients with heart disease. - Calcium Channel Blockers:
Sometimes used in specific arrhythmia cases.
Catheter Ablation
For frequent or life-threatening V Tach, doctors may recommend ventricular tachycardia ablation. This minimally invasive procedure targets and destroys the tissue responsible for the abnormal electrical signals.
Ventricular Tachycardia Ablation Success Rate:
Recent studies show that catheter ablation has a success rate of around 70-80% in controlling V Tach, especially in patients with structurally abnormal hearts.
Implantable Cardioverter-Defibrillator (ICD)
An ICD is a device implanted under the skin that detects abnormal ventricular rhythms and delivers shocks to restore normal rhythm. ICDs are life-saving for people at high risk of sudden cardiac death.
The Role of Continuous Monitoring
Continuous monitoring plays a pivotal role in diagnosing and managing ventricular arrhythmias. Unlike standard ECGs that capture a snapshot in time, ECG monitors that record continuously over many hours or days, provide high-fidelity ECG to doctors, thereby enabling them to detect:
- PVC patterns
- V Tach episodes
- Irregular heartbeats that are symptomless
These devices also empower patients by providing near-real-time insights into their heart health, ensuring that erratic heart rhythms don’t go unnoticed.
Prevention and Risk Reduction
While some ventricular arrhythmias are unavoidable due to genetics or prior heart damage, you can take steps to reduce your risk:
- Maintain a heart-healthy lifestyle
- Treat high blood pressure and cholesterol
- Avoid stimulant drugs and excessive caffeine
- Manage sleep apnea
- Follow your doctor’s advice if you have known heart diseases
- Follow an appropriate exercise plan
When to See a Specialist
If you’ve experienced symptoms like palpitations, dizziness, or episodes where my heart feels like it is racing, it’s crucial to consult a healthcare provider. A ventricular tachycardia specialist or electrophysiologist can help determine the cause and recommend the best treatment path.
Final Thoughts
Ventricular arrhythmias are more than just uncomfortable sensations – they can be serious indicators of underlying heart rhythm problems. From premature ventricular complexes to life-threatening V Fib, these conditions require prompt attention, proper diagnosis, and often long-term management.
With advancements in irregular heartbeat monitor technology, patients and physicians now have better tools to detect, monitor, and treat these rhythms early – before they lead to serious complications.
FAQs: Ventricular Arrhythmias
Q: What’s the difference between V Tach and V Fib?
A: In V Tach, ventricles contract in a coordinated manner but do so very rapidly. In V Fib, ventricles contract in an uncoordinated manner.
Q: What is the success rate of V Tach ablation?
A: Ventricular tachycardia ablation has a success rate of 70-80% for reducing arrhythmia episodes.
Q: How do I know if my rapid heartbeat is dangerous?
A: Persistent sudden rapid heartbeat with symptoms like fainting or chest pain requires immediate medical attention.
If you’re concerned about ventricular arrhythmias, talk to your healthcare provider about continuous monitoring options to keep your heart health a priority.