The cruel trick of arrhythmias: silence while you rest, symptoms when you rise.
When it comes to heart health, arrhythmias don’t always follow the rules. At rest, you could be reading a book, working at your desk, or even asleep – yet your heart may be slipping into an irregular rhythm without you realizing it. Later, when you exercise, climb stairs, or push yourself a little harder, that same hidden rhythm can suddenly make itself felt – palpitations, dizziness, or even fainting.
If you’ve ever wondered why your heart skips a beat, why you feel drained for no clear reason, or whether your racing heartbeat is something more than stress, you’re not alone. Many people face these questions without answers.
What an Arrhythmia Really Means for You
An arrhythmia is simply an irregular rhythm of your heartbeat. But “simple” doesn’t mean harmless. Some arrhythmias may cause nothing more than the occasional skipped beat. Others, like atrial fibrillation (AFib) or ventricular tachycardia, carry serious risks.
The most common arrhythmias include:
- Atrial fibrillation (AFib): The most common sustained arrhythmia. You may not feel it, yet it raises your risk of stroke fivefold.
- Supraventricular tachycardia (SVT): A sudden racing heartbeat that can feel alarming, even if brief.
- Ventricular tachycardia (VT): A rhythm disturbance in the heart’s lower chambers that can be life-threatening.
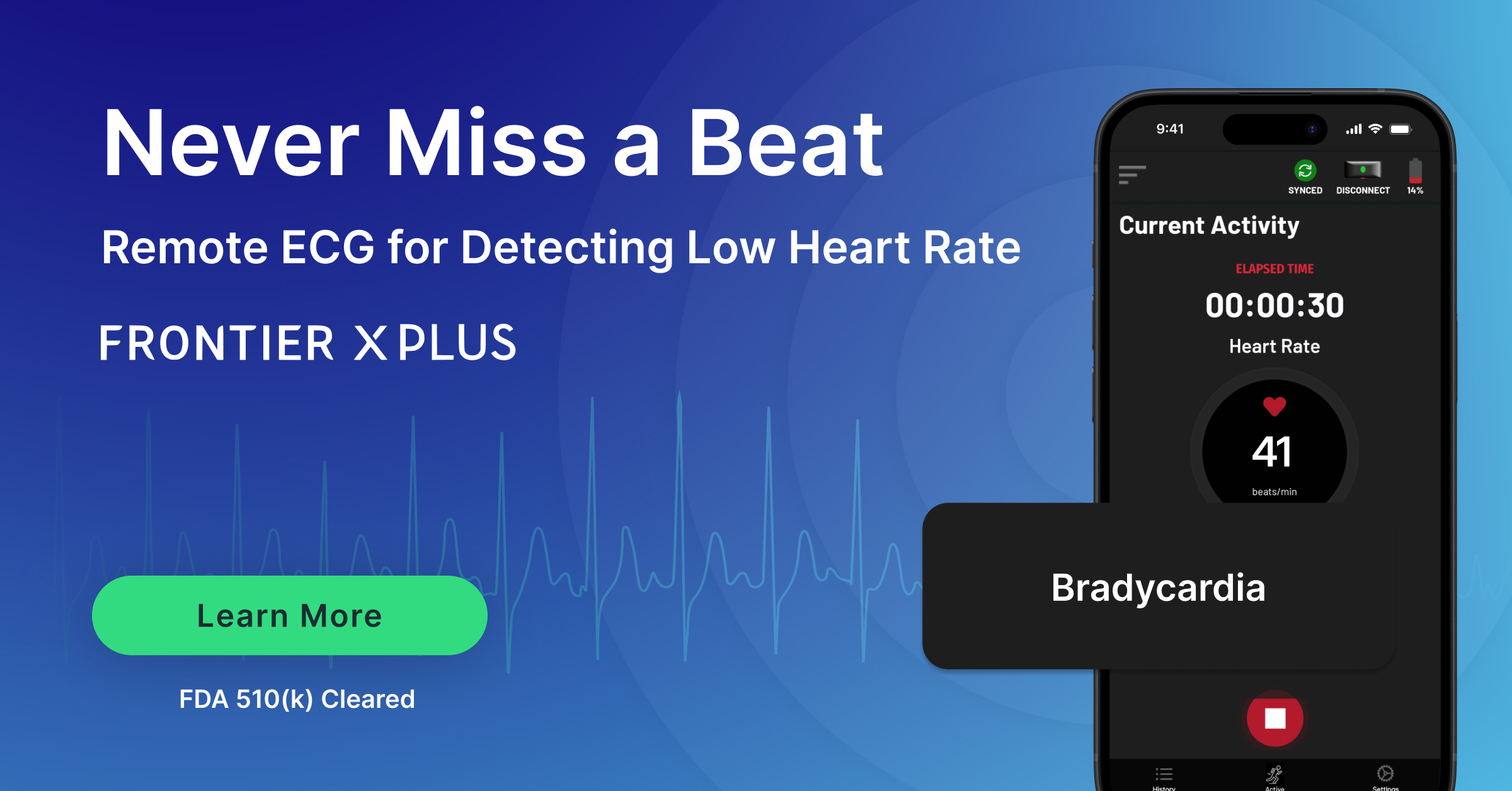
- Bradycardia: When your heartbeat slows too much, leaving you dizzy, faint, or constantly fatigued.
The Silent Arrhythmias You Might Never Notice
The crucial part of some arrhythmias is their occurrence without any symptoms. You may feel perfectly fine, while your heart is misfiring in the background. You might go years without a single symptom, but your risk of stroke or other complications grows quietly in the meantime.
This is especially true with atrial fibrillation. Many people discover it only after a major event. Imagine your heart “screaming” on the inside, but your body giving you no clue. That’s what makes silent arrhythmias so dangerous.
When Symptoms Hit You During Activity
On the flip side, you might feel absolutely normal at rest – only to have symptoms appear during activity. Maybe it’s while jogging, playing a game, or even walking quickly to catch a train. Suddenly, your heart races, your chest feels tight, or you’re left gasping for air. No wonder cases like Juan Izquierdo, the 27-year-old footballer who collapsed during a Copa Libertadores match, resonate so strongly. Despite being diagnosed years earlier with a ‘small arrhythmia,’ he had no symptoms—until exertion pushed his heart into crisis.
These episodes aren’t just unpleasant – they can be dangerous. Exercise-induced arrhythmias, such as ventricular tachycardia, can escalate quickly. If you’ve ever brushed off palpitations or dizziness as “just pushing too hard,” it’s worth taking a closer look.
Why the Typical Tests Often Fail You
Here’s the frustrating part: most medical tests look at your heart for only a short time. A 10-second ECG in your doctor’s office, or even a 24-hour Holter monitor, might completely miss your arrhythmia.
Why? Because your heart may not always misfire when it’s being watched. The skipped beats may happen while you’re asleep, or during a random workout two days later. Short-term checks give you snapshots, but what you need is the full story.
This leaves you with questions:
- Was that flutter I felt just stress – or something serious?
- Am I safe to keep exercising?
- Could I be living with a silent arrhythmia and not know it?
How Continuous Monitoring Changes the Game
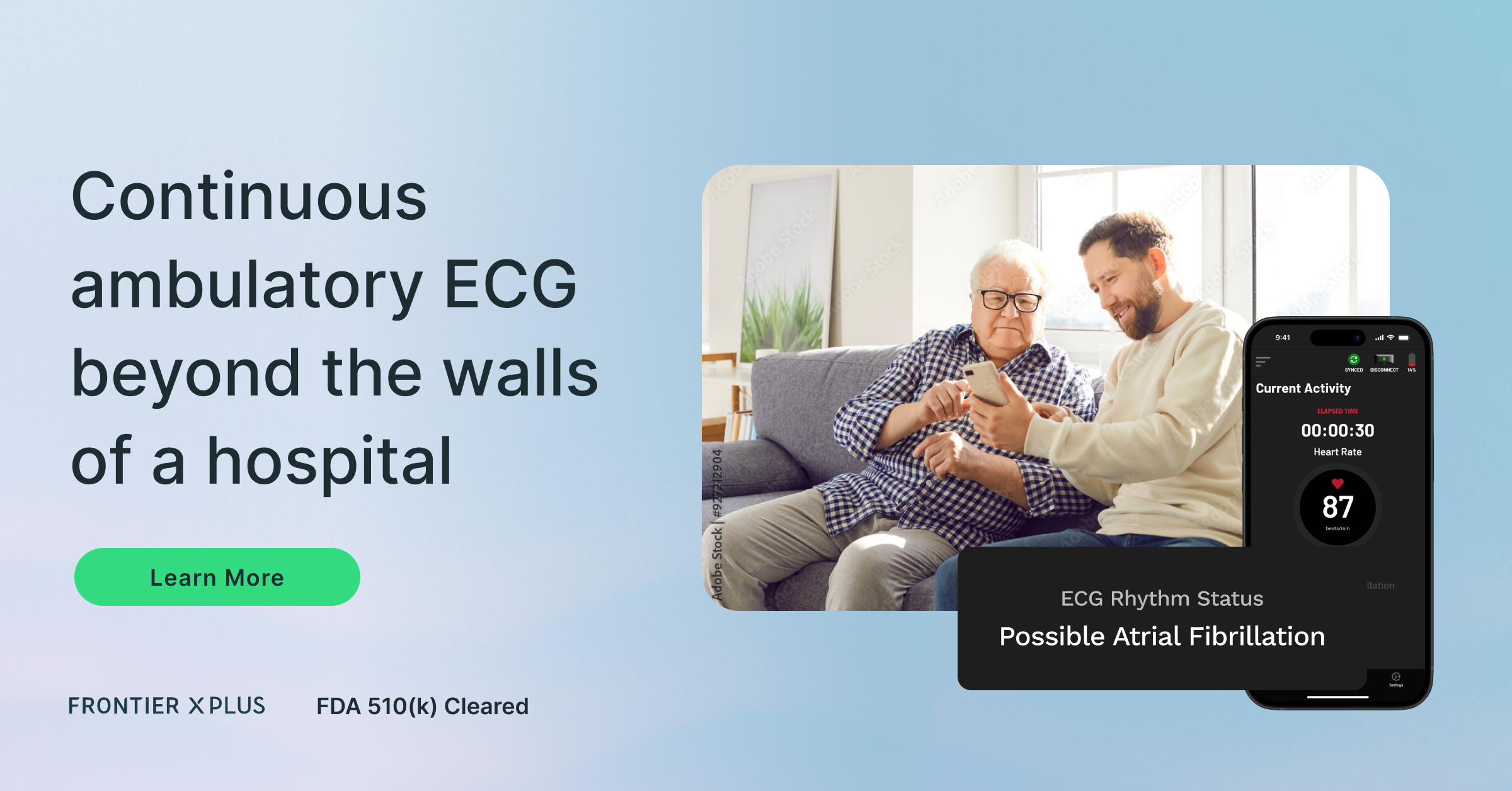
The only way to truly understand your heart is to see what it’s doing across your whole life – not just for a few minutes in a clinic. That’s where ECG monitors that record continuously come in.
With devices like:
- Frontier X Plus (a prescription-based, FDA-cleared device for medical use)
- Frontier X2 (a wellness-focused monitor for athletes and health-conscious individuals)
– you can track your ECG continuously. Whether you’re sitting at your desk, walking your dog, or pushing through a workout, every beat is captured.
For you, this means:
- No more guessing: You’ll know if your dizziness or fatigue is linked to your heart.
- Peace of mind: Silent arrhythmias won’t go unnoticed.
- Better decisions: If you’re an athlete, you can train with confidence. If you’re managing a condition, your doctor can access your data via a cloud and an app and guide treatment.
The Real Risks You Face
Missing arrhythmias comes with a huge cost:
- Silent AFib increases your risk of stroke, even if you never feel a symptom.
- Exercise-induced arrhythmias can trigger sudden cardiac events.
- Quality of life suffers when unexplained fatigue or palpitations leave you anxious.
- Athletes risk pushing their hearts past safe limits without knowing it.
It’s not about fear – it’s about being informed. Your heart shouldn’t be a mystery.
Why You Need to Pay Attention Now
If you’ve ever brushed off chest flutter, ignored fatigue, or chalked up dizziness to dehydration, it may be time to take your heart health seriously. You don’t want to wait until a missed arrhythmia leads to something worse.
The paradox is clear: your heart could be quiet when you expect noise, or noisy when you expect quiet. The only way to know for sure is to listen more closely – every beat, every day.
Join Us Live: Learn From the Experts
This AFib Awareness Month, we’re bringing you insights from two leading Cleveland Clinic cardiologists:
Silent to Symptomatic: Arrhythmias Across Daily Life and Exercise
Thursday, September 25, 2025
9:00–10:00 AM EDT
6:30–7:30 PM IST
Speakers
- Dr. Niraj Varma – Professor of Medicine, Section of Electrophysiology and Pacing, Cleveland Clinic
- Dr. Tamanna Singh – Co-Director, Sports Cardiology Center, Cleveland Clinic
They’ll break down how arrhythmias appear in rest vs exercise, what you need to watch for, and how continuous monitoring can protect your heart.
FAQs on Arrhythmias and Heart Health
Q1. Could I really have an arrhythmia without knowing it?
Yes. Many arrhythmias, especially atrial fibrillation, can be silent. You may feel perfectly fine while your heart is in an irregular rhythm.
Q2. What symptoms should I watch out for?
Pay attention to palpitations, chest flutter, dizziness, fainting, unexplained fatigue, or shortness of breath. These may be signs of an irregular heart arrhythmia.
Q3. What are the most common arrhythmias?
The most common include atrial fibrillation, supraventricular tachycardia, ventricular tachycardia, and bradycardia.
Q4. How are arrhythmias treated?
Treatment depends on the type. It may involve medication, ablation procedures, implantable devices, or lifestyle adjustments.
Q5. Why is atrial fibrillation so serious?
Because it raises your risk of stroke. Even if you never feel symptoms, AFib can cause clots that travel to the brain.
Q6. How does long-termECG monitoring help me?
It captures your heartbeat during your real life – while you rest, work, and exercise. This way, silent arrhythmias don’t go unnoticed, and symptomatic ones are tracked with context.
Q7. Should I consider long-term monitoring?
If you’ve had unexplained palpitations, fainting, or fatigue – or if you’re an athlete returning to training after a cardiac scare – yes, long-term monitoring may be right for you.
Final Takeaway
Your heart doesn’t always play by the rules. It can be silent when you expect noise, and noisy when you expect silence. That paradox makes arrhythmias easy to miss – but dangerous to ignore.
With long-termECG monitoring and expert care, you can finally uncover what your heart is really doing. Don’t wait for symptoms to decide your future – listen to your heart now.
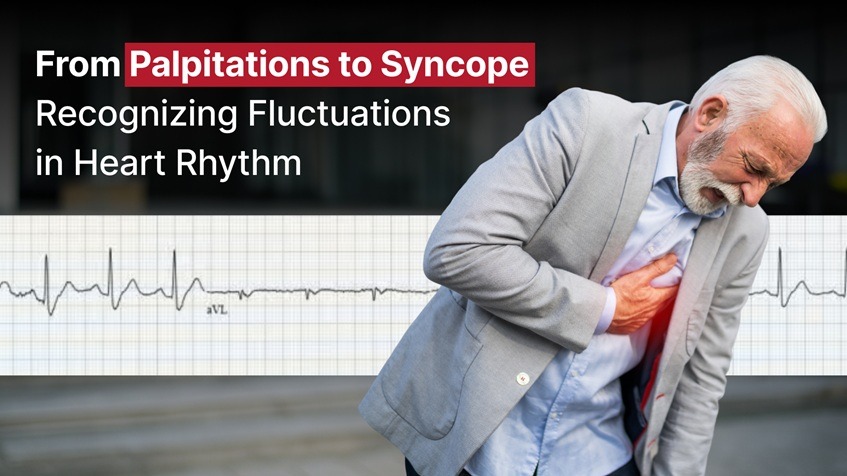
Our hearts beat thousands of times per day, a rhythmic cadence that most of us never notice. But for some, that cadence occasionally stumbles, quickens, or falters. These irregularities in heart rhythm can manifest as palpitations or even lead to sudden episodes of fainting, known as syncope. Understanding what these symptoms mean and when they warrant medical attention is crucial for protecting your cardiovascular health.
In this blog, we’ll explore the spectrum of heart rhythm abnormalities – from harmless skips to potentially serious arrhythmias – and explain how long-term ECG monitoring can play a vital role in early detection and prevention.
What Are Palpitations?
Palpitations are sensations of a rapid, fluttering, or pounding heart. Some people describe them as skipped beats or a flip-flop feeling in the chest. These sensations can occur during physical activity, emotional stress, or even while at rest.
Common Causes of Palpitations:
- Premature atrial or ventricular contractions (PACs or PVCs)
- Anxiety or panic attacks
- Caffeine or stimulant intake
- Dehydration or electrolyte imbalance
- Thyroid disorders
- Anemia or low blood pressure
In many cases, palpitations are benign and don’t indicate a serious problem. However, persistent or recurrent palpitations may signal a more serious underlying arrhythmia.
When Palpitations Are a Warning Sign
While occasional palpitations can be harmless, certain red flags increase the likelihood that they are associated with a cardiac rhythm disorder:
- Palpitations accompanied by dizziness or fainting
- Chest pain or shortness of breath
- Palpitations that last more than a few minutes
- A resting heart rate above 100 bpm without clear cause
If you experience any of the above, it’s essential to seek evaluation. These could indicate supraventricular tachycardia (SVT), atrial fibrillation (AFib), or ventricular tachycardia (VT) – conditions that may require treatment.
What Is Syncope?
Syncope is the medical term for a temporary loss of consciousness, commonly referred to as fainting. It occurs when there is a sudden drop in blood flow to the brain. While syncope can be caused by non-cardiac conditions (like a vasovagal response or dehydration), cardiac syncope is often the most concerning.
Cardiac Causes of Syncope:
- Arrhythmias (bradycardia, tachycardia, pauses)
- Structural heart disease (aortic stenosis, hypertrophic cardiomyopathy)
- Heart block (electrical conduction delays)
- Prolonged QT syndrome
Sudden syncope without warning – especially during exercise or while lying down – is more likely to be cardiac in nature and should never be ignored.
The Spectrum of Heart Rhythm Abnormalities
Understanding where your symptoms fall on the arrhythmia spectrum can help guide evaluation and treatment:
1. PACs and PVCs
These are early beats that originate in the atria or ventricles. They often feel like a skipped or extra beat and are usually benign unless frequent or occurring in a pattern.
2. Sinus Tachycardia
An elevated heart rate due to physiological triggers like exercise, anxiety, or fever. While not an arrhythmia per se, persistent sinus tachycardia may require investigation.
3. Atrial Fibrillation
A chaotic rhythm originating in the atria that leads to an irregular and often rapid heartbeat. AFib is a common cause of palpitations and increases stroke risk.
4. SVT (Supraventricular Tachycardia)
Sudden episodes of fast heart rate that often begin and end abruptly. SVT can cause palpitations, chest discomfort, and even syncope.
5. Ventricular Tachycardia (VT)
A potentially life-threatening rhythm originating in the ventricles. Symptoms include palpitations, dizziness, and syncope.
6. Bradycardia and Heart Block
Slow heart rhythms, often due to conduction system dysfunction. May lead to fatigue, dizziness, or syncope.
Why Timing and Pattern Matter
One of the challenges in diagnosing arrhythmias is their episodic nature. You may experience symptoms only a few times a week, or during sleep or exercise, making them hard to catch with a standard spot check ECG or even a short-term Holter monitor.
How Long-Term ECG Monitoring Helps
Long-term ECG monitors allow for long-duration recording of heart rhythm data. These devices are typically worn on the chest and are capable of capturing both normal and abnormal rhythms over days or weeks. Here’s how they help:
- Catch intermittent arrhythmias missed by standard ECGs
- Correlate symptoms (like palpitations or dizziness) with rhythm data
- Aid physicians in diagnosis and treatment planning
- Provide a timeline of events for better pattern recognition
ECG monitoring is especially valuable for individuals with unexplained syncope, palpitations, or those at high risk for arrhythmias due to family history or underlying cardiac conditions.
When Should You Be Concerned?
Here are some situations where ECG monitors could be life-saving:
- Frequent palpitations with no clear trigger
- Family history of sudden cardiac death
- Fainting during exercise or while lying down
- Heart rate that spikes or drops without exertion
- Known arrhythmia being treated with medications
Working with Your Doctor
Symptom diaries, paired with continuous ECG reports, give cardiologists or electrophysiologists a more complete picture. These tools allow them to:
- Diagnose arrhythmias more accurately
- Assess treatment efficacy
- Decide if interventions like ablation or pacemaker implantation are necessary
Conclusion: Don’t Dismiss the Flutter
Palpitations and syncope can range from harmless to serious. What makes them dangerous is unpredictability and the difficulty of diagnosing the underlying cause based on a short clinical snapshot. That’s why long-term ECG monitoring is a game changer.
If you’ve ever wondered whether that skipped beat was something more, or if you’ve felt dizzy or blacked out without explanation, don’t wait. Consult a medical professional, discuss monitoring options, and take charge of your heart health today.
Because when it comes to your heart, every beat matters.
Your heart is the engine of your body, tirelessly pumping blood and sustaining life. But when its rhythm is disrupted, especially in the form of tachycardia – an abnormally fast heartbeat – it can become more than just a flutter. Two major types of tachycardia include Supraventricular Tachycardia (SVT) and Ventricular Tachycardia (VT), each with distinct causes, implications, and treatments.
In this blog, we explore the difference between SVT and VT, their symptoms, risks, and how continuous ECG technology and modern treatment options are revolutionizing diagnosis and care.
What is Supraventricular Tachycardia (SVT)?
SVT refers to any tachyarrhythmia originating above the ventricles, typically in the atria (the upper chambers), but not originating in the sinoatrial node. These arrhythmias result in a heart rate that can soar to 150-220 beats per minute. SVT rhythm is usually regular; exceptions include atrial fibrillation (AFib) and multifocal atrial tachycardia (MAT).
Types of SVT:
- Atrial Flutter
- Atrial Fibrillation
- Premature atrial contractions (PACs)
- Focal atrial tachycardia
- Multifocal atrial tachycardia (MAT)
- Atrioventricular nodal reentrant tachycardia (AVNRT)
- Atrioventricular reciprocating tachycardia (AVRT)
Symptoms of SVT can be:
- Palpitations
- Lightheadedness
- Shortness of breath
- Chest discomfort
- Fatigue or anxiety
Triggers can be:
- Excess caffeine or alcohol
- Stress
- Sleep deprivation
- Certain medications
Read More: Understanding Supraventricular Tachycardia (SVT): Symptoms, Causes, and Treatment
What is Ventricular Tachycardia (VT)?
VT is a rapid heart rhythm that originates in the ventricles. Unlike SVT, VT can be considered as life-threatening because it affects the heart’s main pumping chambers. Left ventricular tachycardia, in particular, can severely reduce cardiac output, leading to dizziness, fainting, and even sudden cardiac arrest.
Types of VT:
- Sustained VT
- Non-sustained VT
- Monomorphic VT (consistent rhythm)
- Polymorphic VT (variable rhythm)
Common Symptoms can be:
- Dizziness
- Syncope (fainting)
- Weak pulse or no pulse
- Sudden cardiac arrest
Risk Factors can be:
- Previous heart attack
- Heart failure
- Dilated cardiomyopathy
- Congenital heart disease
VT causes most cases of sudden cardiac death, with an estimated rate of 300,000 deaths each year in the United States.
Read More: What is Ventricular Tachycardia and What Are The Most Common Signs?
Comparing SVT and VT: What Sets Them Apart?
| Feature | Supraventricular Tachycardia (SVT) | Ventricular Tachycardia (VT) |
| Origin | Above the ventricles | Within the ventricles |
| Heart Rate | 150-220 bpm | Often >100 bpm |
| Severity | rarely dangerous, unless they stay in SVT for too long | Potentially life-threatening |
| Common Triggers | Stress, caffeine, stimulants | Structural heart disease |
| Treatment Options | Vagal maneuvers, drugs for SVT, SVT ablation | VT drugs, defibrillation, VT ablation |
| Detection | ECG, Holter monitor | ECG, Holter monitor |
Why Does Differentiation Matter?
Correctly identifying whether a fast heart rhythm is SVT or VT can drastically change the course of treatment. Treating VT as SVT can delay life-saving interventions. On the other hand, overtreating SVT as a life-threatening emergency can cause unnecessary stress and medical procedures.
Both conditions require expert diagnosis, but the consequences of mismanagement differ greatly. Continuous heart monitoring is pivotal for capturing these arrhythmias, especially when they are intermittent or asymptomatic.
How Are These Conditions Diagnosed?
The first step is a 12-lead ECG, but due to the fleeting nature of SVT and VT episodes, continuous heart monitoring using medical Holter monitors or advanced wearable monitors provides invaluable insight.
Additional diagnostic tools include:
- Echocardiogram (to assess heart structure)
- Stress tests (to provoke arrhythmia under observation)
- Electrophysiology studies (to map abnormal electrical pathways)
Tests for SVT may involve:
- Event monitors
- Implantable loop recorders
- SVT monitors with patient-triggered symptom tagging
- If symptoms occur under exertion, exercise stress tests will often be ordered to look for these conditions
Treatment Pathways
SVT Treatment Options may be
- Vagal maneuvers as advised by doctors
- Medical treatment for SVT: Beta-blockers, calcium channel blockers
- Drugs for SVT as prescribed by your doctor
- SVT ablation: Catheter ablation procedures targeting the electrical misfiring
- Supraventricular tachycardia catheter ablation: High success rates and often considered first-line for recurrent episodes
Ventricular Tachycardia Treatment may be
- Drugs for VT as prescribed by your doctor
- Ventricular tachycardia treatment drugs: Antiarrhythmic agents tailored to the patient’s heart condition
- Implantable cardioverter-defibrillator (ICD): For high-risk patients
- Ventricular tachycardia ablation success rate: Can reach 70-90% depending on the heart’s structural integrity and underlying cause
- Emergency defibrillation: In cases of pulseless VT
Disclaimer: Medication should be based on a patient’s medical history, current medications, and other patient factors.
Role of Continuous Heart Monitoring
Early detection is essential. Symptoms can be misleading, and many arrhythmias are asymptomatic, especially in early stages.
With continuous heart monitoring:
- Episodes are captured in real-time, even while sleeping or exercising
- Heart rhythm monitors provide a full picture of both SVT and VT frequency
- Data-driven treatment becomes possible, improving outcomes

Prevention and Risk Reduction
While not all cases of SVT or VT are preventable, you can reduce your risk with healthy lifestyle choices and medical supervision:
Prevention Tips:
- Maintain a healthy weight and blood pressure
- Limit caffeine and alcohol
- Manage stress with mindfulness or therapy
- Avoid recreational drugs and smoking
- Get regular exercise, approved by your doctor
- If you have a family history, consider genetic testing or early screening
Final Thoughts
SVT and VT are both forms of tachycardia, but the stakes and strategies involved in treating them are different. The health of the heart depends not just on its strength but also on its rhythm.
Whether you’re managing an SVT heart condition or facing the risks of VT, timely diagnosis, continuous heart monitoring, and appropriate treatments are critical. From vagal maneuvers for SVT to ventricular tachycardia treatment drugs, modern medicine offers effective pathways to manage both.
ECG monitors that can record continuously have transformed the landscape for patients and clinicians alike – offering an accessible, non-invasive window into the heart’s electrical activity in real time.
FAQs
-
What is the main difference between SVT and VT?
SVT originates above the ventricles (usually in the atria), while VT originates in the ventricles. SVT is generally less dangerous than VT, which can lead to sudden cardiac arrest.
-
Can SVT turn into VT?
Not directly. However, individuals with predisposing conditions could experience both types of arrhythmias.
-
Is VT always life-threatening?
No, but sustained VT is a medical emergency and can lead to cardiac arrest if not treated immediately.
-
What are the treatment success rates for VT ablation?
Depending on the cause and patient profile, VT ablation success rates have been over 75%.
-
What is the best monitor to detect SVT or VT at home?
Continuous ECG monitors or medical Holter monitors are the most effective tools for detecting intermittent arrhythmias like SVT and VT.
-
Are there medications available for SVT and VT?
Yes. Drugs like adenosine and beta-blockers are used for SVT, while amiodarone and lidocaine are common for VT (Disclaimer: medication should be based on a patient’s medical history, current medications, and other patient factors)
-
What are vagal maneuvers?
Simple actions like coughing or bearing down can help interrupt SVT episodes and restore normal rhythm.
-
Can I live a normal life with SVT or VT?
With proper treatment and monitoring, many individuals with these arrhythmias can lead normal, active lives.
Have you ever checked your pulse and found it unusually slow, especially after a workout or first thing in the morning? For athletes and fitness enthusiasts, a resting heart rate(RHR) below 60 beats per minute (bpm) might be completely normal. But for others, it could be a warning sign. So how do you know whether a slow heart rate is healthy or something more serious?
In this blog, we’ll break down the differences between athletic bradycardia, sinus bradycardia, and general bradycardia, and explain how ECG monitoring with a tool like the FDA-cleared Frontier X Plus can help you stay confident and safe.
What Is Bradycardia?
Bradycardia is the clinical term for a heart rate below 60 bpm in adults. While that may sound concerning, it’s not always dangerous. Many people — especially trained athletes — naturally have a slower resting heart rate because their hearts are more efficient at pumping blood.
But not all bradycardia is created equal.
1. Athletic Bradycardia: A Sign of a Strong Heart
If you’re a runner, cyclist, swimmer, or just very active, you may notice that your RHR is below the range of 60 to 80 bpm for the average adult; a young, healthy athlete may have a heart rate of 30 to 40 bpm. This is called athletic bradycardia.
- Cause: Long-term endurance training boosts the strength of the heart muscle and increases vagal tone, which slows the heart rate.
- Rhythm: Normal sinus rhythm — just slower.
- Symptoms: None — athletes usually feel great.
This type of bradycardia is normal, harmless, and even desirable in the athletic population.
2. Sinus Bradycardia: When Slowness Starts at the Source
Sinus bradycardia refers to a slow heart rate caused by the sinoatrial (SA) node, your heart’s natural pacemaker. It may occur in people during sleep, at rest, or as a side effect of medications (like beta-blockers).
- Cause: Normal physiology, medications, or medical conditions
- Rhythm: Still a regular sinus pattern, but slow
- Symptoms: May be asymptomatic or cause fatigue, lightheadedness, or fainting
Sometimes normal, sometimes a signal for further evaluation — especially if symptoms are present.
3. Concerning Bradycardia: When Slow Is a Red Flag
Not all slow heart rhythms come from the SA node. Bradycardia may also result from electrical signal blockages in the heart, such as AV block or junctional rhythms. These cases often require intervention.
- Cause: Heart disease, aging, or damaged electrical pathways
- Rhythm: Irregular or abnormal patterns (not sinus)
- Symptoms: Fatigue, fainting (syncope), dizziness, confusion
These forms of bradycardia should be taken seriously and evaluated by a cardiologist.
Why It’s Hard to Tell the Difference
If you’re healthy and active, it’s easy to dismiss a slow heart rate as part of your fitness gains. But what if you’re not sure? Or what if symptoms show up during rest, sleep, or exercise? Traditional ECGs or smartwatches don’t give you the whole picture — especially if symptoms are intermittent.
That’s where ECG monitors become invaluable.
Read More : How Frontier X Plus is Better Than a Smartwatch for Heart Monitoring
ECG monitors: Your Ally in Understanding Heart Rhythms
Prescription-based, chest-worn ECG monitors that record continuous heart data — including sinus rhythm, arrhythmia, tachycardia, and bradycardia episodes — while you go about your day or even during workouts and sleep, help in many ways:
- Continuously capture full ECG waveforms for up to 24 hours per hour of charge, unlike 30-second smartwatch recordings
- Label periods of activity and rest, helping distinguish between athletic and pathological bradycardia
- Provide end-of-study ECG reports for clinical review
- Help your doctor understand the cause, context, and clinical relevance of slow heart rhythms
Whether you’re training hard or managing symptoms, ECG monitors help answer the crucial question: Is my slow heart rate a sign of strength — or something sinister?
Who Should Consider Monitoring?
- Endurance athletes wanting reassurance
- People with symptoms like dizziness, fatigue, or fainting
- Individuals taking medications that affect their heart rate
- Anyone with a history of cardiovascular arrhythmia or abnormal heart rhythm
- Patients post-procedure (like ablation or pacemaker placement)
Final Thoughts
Bradycardia — a slow heart rate typically defined as fewer than 60 beats per minute — isn’t always a warning sign. In fact, for athletes and fitness-conscious individuals, it’s often a reflection of an efficient, well-conditioned heart. A low resting heart rate can indicate cardiovascular health and endurance, rather than dysfunction.
At the same time, effective tramadol pain relief can indirectly benefit the cardiovascular system, since untreated chronic pain is associated with increased stress and sympathetic activation, which burden the heart (https://doctorsmileonline.com/pain-tramadol/).
However, context matters. When bradycardia is unexplained, intermittent, or accompanied by symptoms such as fatigue, dizziness, chest discomfort, or fainting, it may indicate an underlying issue, such as sinus node dysfunction, AV block, or the effects of certain medications. In older adults or those with heart disease, it may even be an early marker for conduction system problems requiring medical attention.
This is precisely where ECG monitoring becomes essential. Rather than relying on isolated clinic-based ECGs that often miss transient episodes, ECG monitors offer:
- Extended rhythm tracking during daily activities, rest, and exertion
- Real-time correlation between symptoms and heart events through tagging features
- A professional review that filters out benign findings from clinically significant arrhythmias
With these insights, you and your physician can make informed decisions, identifying whether a slow rhythm is a natural outcome of fitness or a signal that further evaluation is warranted.
So whether you’re a triathlete training for your next competition, someone recovering from a cardiac event, or simply proactive about your cardiovascular health, continuous ECG devices offer clarity, confidence, and peace of mind. They transform vague symptoms into actionable data, empowering you to take control of your heart health with precision and assurance.
You’re sitting quietly — watching TV, reading, or lying in bed — and suddenly, your heart flutters. It skips. It races. The episode lasts just a few seconds, maybe a minute, and then it vanishes like it never happened.
You go to the doctor. They run a 12-lead ECG. Maybe even a 24-hour Holter test.
The results? “Normal.”
But what you felt was real. So why didn’t the test catch it?
The Mystery of “Normal” Test Results
Many people who experience occasional palpitations—sudden thuds, flips, or rapid beats—are told that their hearts are perfectly fine. For some, that’s comforting. For others, it’s frustrating, especially when the symptoms continue.
The truth is, standard heart tests often miss intermittent arrhythmias. If your heart rhythm disturbance doesn’t occur during the short monitoring window, the ECG will appear normal. It’s like trying to catch a lightning strike with a snapshot, while we need a CCTV camera.
Why Short-Term ECGs Aren’t Always Enough
A standard ECG records your heart’s electrical activity for a few seconds. A Holter monitor might capture 24 to 48 hours. But what if your palpitations show up once a week? Or once a month? Or only at night? In these cases, standard tests can easily miss rhythm disturbances that may cause palpitations
Not all palpitations are created equal. Some represent harmless irregularities, while others may signal more serious electrical instability in the heart. The following are common rhythm disturbances that can cause fluttering, skipped beats, or pounding sensations, often transient and missed in standard ECGs:
- Paroxysmal Atrial Fibrillation (AFib): These are short-lived episodes of atrial fibrillation that come and go unpredictably, often lasting minutes to hours and stopping on their own without treatment. Because they’re intermittent and may not cause overt symptoms, paroxysmal AF can go undiagnosed for years, despite significantly increasing stroke risk over time.
- Premature Atrial Contractions (PACs) and Premature Ventricular Contractions (PVCs): These are early beats originating in the atria or ventricles. While they’re usually benign, frequent PACs or PVCs can cause noticeable palpitations or a feeling of a skipped heartbeat. In some cases, especially when very frequent, they may be associated with structural heart disease or contribute to cardiomyopathy.
- Supraventricular Tachycardia (SVT): SVT refers to a group of arrhythmias that start in the atria and cause sudden-onset, fast heart rhythms — often described as a rapid, pounding sensation in the chest. Episodes may last seconds to hours and can terminate spontaneously. While often not life-threatening, recurrent SVT can significantly impair quality of life and may require intervention if it is frequent.
- Atrial Flutter: Similar to AFib, this arrhythmia involves rapid electrical activity in the atria but in a more organized, cyclical pattern. It may present with a fast, regular rhythm and is often associated with symptoms like fatigue or breathlessness. Atrial flutter is frequently seen in patients with structural heart disease or post-ablation AF recurrence.
- Ventricular Arrhythmias: While rare in healthy individuals, arrhythmias like ventricular tachycardia (VT) or ventricular fibrillation (VF) are more serious and potentially life-threatening. Occasional ventricular ectopy (i.e., isolated PVCs) is common and benign, but sustained or frequent runs — particularly during exertion or in people with structural heart disease — warrant immediate investigation.
Even serious heart rhythm irregularities can go undetected if they don’t occur during the test.
Read More: Monitoring Asymptomatic Atrial Fibrillation With The Frontier X Plus
But If It’s Infrequent, Should You Worry?
Yes — and here’s why.
Palpitations might seem benign, especially if they’re rare or go away quickly. But even occasional or “silent” episodes can be early warning signs of more serious conditions. Some possibilities include:
- Atrial fibrillation (AF), especially the paroxysmal kind, which often starts intermittently before becoming persistent
- Tachycardias that could increase in frequency or duration over time
- Heart failure risk, if arrhythmias disrupt blood flow long-term
- Stroke risk, particularly from undiagnosed AF, even without symptoms
Studies show that around one-third of those with AFib may not experience symptoms. So occasional flutters shouldn’t be ignored, especially if you have risk factors like high blood pressure, diabetes, or a family history of heart disease.
What Does a Palpitation Actually Feel Like?
Patients describe them in different ways:
- “It felt like my heart skipped a beat.”
- “It was fluttering in my chest for a few seconds.”
- “My heart pounded out of nowhere.”
- “There was a thud, then a pause.”
Sometimes the flutter is followed by dizziness, fatigue, anxiety, or a brief sense of breathlessness. These signs matter. They could be clues to underlying cardiovascular arrhythmias, not just stress or overexertion.
The Role of Continuous ECG Monitoring In Managing Heart Health
This is where continuous, long-term ECG monitoring fills the gap. Unlike traditional tools, these devices are worn for days or even weeks. They:
- Track your heart 24/7, even while you sleep, work out, or rest
- Capture rare and unpredictable events that standard ECGs miss
- Allow symptom tagging, so you can mark when you feel something off
- Record high-fidelity data across all daily activities
The key is remote monitoring, letting your physician review real-time ECG data from your device, sometimes with cloud-based storage and alerts for irregularities.
This means that even one-off flutters, short AF episodes, or infrequent PVCs can be caught and reviewed, giving your care team a full picture of your sinus rhythm and any deviations from it.
What Happens After the Data Is Captured?
Once the ECG data is collected:
- Cardiologists analyze the pattern, timing, and frequency of irregularities.
- They look for heart arrhythmias, prolonged QT intervals, abnormal beats, or signs of AF heart rhythm.
- Based on the findings, they may recommend treatment (medications, ablation), further testing, or lifestyle changes.
Importantly, long-term monitors provide insight into when the problem happens, such as during stress, after meals, or at night, which helps tailor both diagnosis and treatment.
When Should You Consider Continuous Monitoring?
You might benefit from long-term ECG tracking if:
- You feel fluttering, skipping, pounding, or irregular beats occasionally
- You’ve had normal tests but persistent symptoms
- You experience dizziness, fatigue, chest discomfort, or breathlessness without explanation
- You’re monitoring the effects of medications or post-ablation outcomes
- You have a family history or risk factors for arrhythmias or AF
Final Thoughts: Don’t Dismiss the Flutters
Just because a quick test comes back normal doesn’t mean your heart is behaving normally all the time. Heartbeat arrhythmias can be elusive; they may hide for days, only to show up when you’re not looking. Remote, continuous ECG monitoring empowers you and your doctor to detect hidden issues, uncover patterns, and start treatment early. So, the next time your heart flutters, don’t ignore it. Listen closely. If needed, track it. And give your heart the attention it deserves.
Premature Ventricular Contractions (PVCs) are early, extra heartbeats that start in the heart’s lower chambers (the ventricles), disrupting the heart’s normal rhythm for a moment. They are relatively common in 3% to 20% of the general population and are often detected during evaluations for palpitations or incidentally on routine electrocardiograms (ECGs). They often show no symptoms and require no special treatment. But for some, these contractions can cause uncomfortable sensations, and anxiety, or even signal an underlying cardiac problem. Let’s first understand what PVCs are and then discuss everything you need to know about them.
What are PVCs?
PVC is short for Premature Ventricular Contractions. They are also called Ventricular premature beats and Ventricular extrasystoles. In a normal, synchronized heart rhythm, your heart beats in a smooth, steady rhythm thanks to a natural electrical system. It all starts in a small area called the sinoatrial (SA) node, located in the upper right part of your heart. This is your heart’s natural pacemaker — it sends out a signal that tells the top chambers (the atria) to contract and push blood into the lower chambers (the ventricles).
Next, the signal passes through a checkpoint called the atrioventricular (AV) node, which briefly slows things down to give the ventricles time to fill with blood. Then the signal travels down special pathways to the bottom of the heart, making the ventricles contract and pump blood to the lungs and the rest of your body.
But sometimes, things don’t go as planned. In a condition called Premature Ventricular Contractions (PVCs), the signal starts too early, and it comes from the bottom chambers (the ventricles) instead of the top. This early signal can throw off the heart’s normal rhythm, leading to a feeling of a skipped or extra beat. You might feel them as a flutter in the chest, a missed beat, a strong thump, or a momentary pause in your heartbeat
Most PVCs are harmless, especially in individuals with healthy hearts. But in some cases, they may reflect or contribute to heart dysfunction, especially when they occur frequently.
What PVCs Feel Like: Common Symptoms
If you have PVC, you may or may not feel the symptoms. You may discover them only during a routine ECG or check-up. When symptoms do occur, they can include:
- A sensation of skipped or irregular heartbeats
- Chest fluttering
- Chest Thumping,
- Lightheadedness
- Fatigue and mild shortness of breath.
It is necessary to contact your healthcare professional if you have symptoms like fainting.
What Causes PVCs?
PVCs can occur in healthy individuals without any clear reason. However, several triggers and risk factors have been associated with their occurrence.
1. Lifestyle and Non-Cardiac Triggers
Certain daily practices, habits, or conditions that are not directly related to the heart can trigger PVCs. Here are some common triggers:
- Caffeine
- Alcohol
- Tobacco use
- Stress and anxiety
- Sleep deprivation
- Medications (like decongestants or asthma medications)
2. Medical Conditions
Pre-existing medical conditions can trigger PVCs. Here are a few triggers:
- Electrolyte imbalances (low potassium, magnesium, or calcium)
- Anemia
- High blood pressure
- Structural heart disease (like cardiomyopathies or valve disorders)
- Acute events such as heart attacks or myocarditis
PVCs can also occur more frequently with age. Males, African Americans, and individuals with hypertension or bundle branch block are statistically more prone to developing PVCs.
Understanding the risks of PVC
In healthy individuals, occasional PVCs are generally not dangerous. However, their impact depends on several factors, including frequency, symptoms, and underlying heart health.
- Occasional PVCs in healthy individuals are usually benign and don’t require treatment.
- Frequent PVCs (e.g., >10% of total heartbeats in 24 hours) may impair cardiac function.
- Persistent high PVC burden can lead to PVC-induced cardiomyopathy, causing heart muscle weakening and left ventricular dysfunction.
- Nonsustained VT occurs when ≥3 PVCs appear consecutively but resolve within 30 seconds.
- Sustained VT is a serious condition where a rapid heartbeat lasts >30 seconds and may cause syncope or sudden cardiac arrest.
- Symptoms like palpitations, dizziness, or breathlessness alongside PVCs require further clinical evaluation.
- Frequent or symptomatic PVCs should prompt cardiology referral, especially in those with underlying heart disease.
Close Monitoring Needed:
Those with a high PVC burden or preexisting heart conditions need regular follow-ups. Early detection and appropriate management can help reverse damage and significantly improve the quality of life. Continuous ECG monitors can help track PVC burden over time and evaluate treatment effectiveness, especially in individuals at risk of PVC-induced cardiomyopathy.
How Are PVCs Diagnosed?
If you feel unusual heartbeats, your doctor may recommend:
12-lead Electrocardiogram (ECG) – to detect abnormal heartbeats
Holter monitor – a 24 to 48-hour device to track your heart rhythm
Echocardiogram – to check for structural heart problems
Exercise Stress testing – to evaluate how your heart behaves under physical exertion.
Wearable ECG devices – Portable, wearable monitors that continuously track your heart rhythm over days or weeks for irregularities
These tests help rule out underlying heart disease, which is critical in determining if your PVCs are benign or a sign of something more serious.
The Role of Wearable ECG Devices
Recent advancements in FDA-cleared wearable continuous ECG monitors have made it easier to detect both symptomatic and silent PVCs. These devices offer continuous, real-time heart monitoring outside of clinical settings, making it possible to track irregular beats over days or weeks and identify high-burden PVCs that may go unnoticed during short ECGs or clinic visits.
Unlike wrist-based devices or traditional Holter monitors that require periodic clinic visits, patchless, chest-worn, medical-grade, continuous ECG monitors like the Frontier X Plus can capture continuous, high-fidelity ECG waveforms in real time for up to 24 hours (or as long as the clinician prescribes), with just an hour of chargingIt enables remote access to ECG data by physicians for early diagnosis, reducing the need for repeated in-clinic testing. Additionally, detailed ECG reports can be downloaded and easily shared with healthcare providers for follow-up, second opinions, or long-term heart health management.
By integrating seamlessly into daily life, the Frontier X Plus offers high-fidelity continuous ECG recording that can aid physicians in early detection of arrhythmias like atrial fibrillation, as well as ongoing evaluation and treatment planning. While the Frontier X Plus does not detect PVCs directly, the ECG data it captures can be reviewed by physicians to assess rhythm patterns. In patients with a known high PVC burden, this data may support long-term monitoring of treatment effectiveness, lifestyle changes, or outcomes post-catheter ablation, with appropriate clinical oversight.
Read More: Continuous ECG Monitoring to Detect Asymptomatic Heart Arrhythmias During Sleep
How Are PVCs Treated?
Treatment is not always necessary for people with no symptoms and low-frequency PVCs.
What can help?
- Lifestyle changes can help manage PVCs:
- Reduce or avoid caffeine and alcohol
- Get adequate sleep
- Manage stress and anxiety
- Avoid stimulants and certain decongestants
2. Medications may be prescribed if symptoms are bothersome:
- Beta-blockers
- Calcium channel blockers
- Antiarrhythmic drugs (in selected cases)
3. If lifestyle changes and medicines don’t have an effect, radiofrequency catheter ablation may be recommended.
Summary
PVCs are common and often harmless, especially in healthy individuals. However, frequent or symptomatic PVCs can indicate underlying cardiac issues and warrant evaluation. With advanced continuous ECG monitoring, you can take charge of your heart health from the comfort of home.
Whether you’re evaluating palpitations or managing a diagnosed arrhythmia, understanding your heart rhythm is the foundation for peace of mind and proactive care.
FAQs
1. Are PVCs life-threatening?
In most healthy individuals, PVCs are harmless. However, in people with heart disease or very frequent PVCs, they can lead to complications if untreated.
2. Do PVCs require lifelong treatment?
Not always. Many people outgrow them, or they reduce with lifestyle changes. Medications or ablation may be needed in persistent or high-burden cases.
3. Is exercise safe with PVCs?
Generally, yes, especially if you don’t have structural heart disease. Still, consult your healthcare professional before starting a workout routine if you have frequent PVCs.
4. Can I monitor PVCs at home?
No. Wearable ECG monitors like the Frontier X Plus allow users to record their heart rhythm continuously. While the device can detect atrial fibrillation, it does not detect PVCs. To identify PVCs or other irregularities, the recorded ECG data must be reviewed by a physician.
5. Can anxiety cause PVCs?
Yes. Stress and anxiety are common triggers. Learning stress-management techniques may help reduce their frequency.
6. When should I see a doctor about PVCs?
If you feel dizzy, faint, have chest pain, or notice frequent irregular heartbeats, you should see a healthcare provider for evaluation.
When it comes to heart rhythm disorders, atrial flutter (AFL) and atrial fibrillation (AF) are two of the most common – and often confused – conditions. Both can lead to serious health risks, including stroke and heart failure, but understanding how they differ is critical for early detection, effective management, and peace of mind.
In this blog, we’ll break down the differences between atrial flutter and atrial fibrillation, why these arrhythmias matter, and how modern continuous ambulatory monitoring can help you and your healthcare team stay ahead of silent or intermittent episodes.
What Are Atrial Flutter and Atrial Fibrillation?
Atrial flutter and atrial fibrillation are types of supraventricular arrhythmia, meaning they originate in the heart’s upper chambers (atria). Both result in abnormal electrical activity that disrupts normal heartbeat patterns.
Atrial Flutter
- Atrial flutter is characterized by rapid but regular electrical signals in the atria.
- The atria may beat at rates of about 300 beats per minute, but the ventricles (the lower chambers) usually beat at a regular, normal rate.
- On an ECG, atrial flutter often produces a classic sawtooth pattern.
Atrial Fibrillation (AF)
- AF involves chaotic, disorganized electrical signals in the atria.
- The atria quiver instead of contracting effectively.
- Ventricular response is typically irregular and faster than normal.
- On ECG, Atrial Fibrillation presents with the typical narrow complex “irregularly irregular” pattern with no distinguishable P-waves
What Causes These Arrhythmias?
Both conditions share overlapping risk factors:
- High blood pressure
- Diabetes
- Thyroid disorders
- Coronary artery disease
- Heart valve disorders
- Excessive alcohol use
- Sleep apnea
However, atrial flutter is more often linked to scarring in the atria (e.g., after heart surgery), while AFib tends to be associated with age-related atrial changes or a family history of heart disease.
Symptoms: How Do They Feel?
Both atrial flutter and AFib can cause:
- Palpitations (sensation of a racing or fluttering heart)
- Shortness of breath
- Dizziness or lightheadedness
- Chest discomfort
- Fatigue
AFib is often more unpredictable because of its irregular rhythm. Atrial flutter, despite being fast, may feel steadier but can still lead to serious complications like blood clots.
Read More: Preventing Complications from AFib: What You Need to Know
Why Does It Matter?
Stroke Risk
Both arrhythmias allow blood to pool in the atria, increasing the risk of clots that can travel to the brain and cause a stroke. People with AFib have a slightly higher stroke risk, but AFL also demands prompt medical attention.
Heart Failure
Untreated AFib and flutter can weaken the part of the heart responsible for pumping blood, leading to heart failure over time.
Different Treatments
- Atrial flutter treatment often involves catheter ablation, as the abnormal pathway can usually be targeted precisely.
- AFib treatment is more complex, requiring a combination of atrial fibrillation medication, rate or rhythm control strategies, and sometimes ablation.
In both conditions, blood thinners are commonly prescribed to prevent clots. When medication is needed, doctors may use drugs for atrial flutter and AFib, such as beta-blockers, calcium channel blockers, or antiarrhythmics to control the rate or rhythm.
Prevention Tips for Atrial Flutter & Atrial Fibrillation
-
Maintain a heart-healthy diet
Focus on a Mediterranean-style diet rich in fruits, vegetables, whole grains, and lean protein. This supports cardiovascular function and reduces inflammation.
-
Stay physically active
Engage in at least 150 minutes of moderate aerobic exercise weekly to improve circulation and heart rhythm stability.
-
Limit alcohol and caffeine
Excessive intake of stimulants can trigger arrhythmias. Stick to moderation or avoid them altogether if you’re prone to irregular rhythms.
-
Manage chronic conditions
Proper control of hypertension, diabetes, sleep apnea, and thyroid disorders can lower your arrhythmia risk.
-
Avoid smoking
Tobacco use increases your risk of heart disease and rhythm disorders. Quitting has immediate cardiovascular benefits.
-
Monitor your heart rhythm proactively
Use long-term ECG monitors if you’re at risk or symptomatic. Early detection allows early intervention.
-
Routine check-ups and screenings
Especially important if you have a family history of arrhythmia or genetic predisposition. Early screening can prevent complications.
Read More: Healthy Lifestyle Changes for Managing AFib: Tips for Living with Atrial Fibrillation
| Feature | Atrial Fibrillation (AFib) | Atrial Flutter |
| Rhythm | Irregular | Regular |
| Atrial Rate | 100 to 175 bpm disorganised | Up to 300 bpm organized |
| Ventricular Response | Irregular | May be regular or slower than the atria |
| ECG Appearance | No distinct P waves; chaotic baseline | “Sawtooth” pattern |
| Symptoms | Palpitations, fatigue, dizziness, breathlessness | Similar symptoms, sometimes less pronounced |
| Stroke Risk | High | Also elevated, but generally slightly lower than AFib |
| Common Causes | Hypertension, heart disease, thyroid disorders, and alcohol | Same as AFib; often coexists with AFib |
Continuous ECG Technology: Why It’s Critical
One of the biggest challenges is that both arrhythmias can occur intermittently or silently. In fact, people may have episodes of AFib or flutter that they never feel until a complication like a stroke happens.
This is where continuous ECG technology becomes essential:
- It records your heart rhythm around the clock – during work, rest, or exercise.
- It captures both silent and symptomatic arrhythmias that could be missed during short clinic ECGs.
- It helps your doctor decide whether you need an atrial fibrillation medication, a procedure, or simply close follow-up.
Can Atrial Flutter and AFib Coexist?
Yes. Up to half of patients with atrial flutter will eventually develop AFib.
This overlap is important because it can influence your treatment plan. If you’re being evaluated for atrial flutter treatment, your care team will also consider strategies to prevent or manage AFib.
When Should You Seek Medical Advice?
You should speak to a doctor if you experience:
- An irregular or rapid heartbeat at rest
- Shortness of breath or unexplained fatigue
- Dizziness or fainting
- Chest discomfort
If you have risk factors such as high blood pressure, sleep apnea, or a family history of arrhythmias or heart disease, monitoring your heart rhythm proactively can help prevent complications.
Final Thoughts
Understanding the difference between atrial flutter and atrial fibrillation is key to reducing your risk of stroke, heart failure, and other complications. Both conditions can be managed effectively with the right mix of atrial fibrillation medication, drugs for atrial flutter, procedures, and lifestyle changes – but early detection is critical.
Continuous ECG-based heart monitors are valuable tools that help you and your healthcare team detect these arrhythmias before they cause harm, offering clarity and control over your heart health.
About The Frontier X Plus
The Frontier X Plus is an FDA 510(k)-cleared prescription-only medical device offering single-channel ECG monitoring through a comfortable chest-worn design, and can be used continuously for 24 hours between recharges. Built for healthcare professionals, patients with cardiac concerns, and health-focused individuals, it enables early detection of Afib and other irregular heart rhythm analysis, all without wires, adhesives, or hospital visits.
Disclaimer
This content is for informational purposes only and should not be considered medical advice. Always consult a healthcare professional for proper diagnosis and treatment.
FAQs: Atrial Flutter vs. Atrial Fibrillation
Is atrial flutter more dangerous than atrial fibrillation?
Both conditions carry a risk of stroke and heart failure if untreated. AFib generally has a higher stroke risk because of the irregular blood flow, but atrial flutter is also serious and requires medical evaluation.
What is the treatment for atrial flutter?
Common atrial flutter treatment includes catheter ablation, which targets the abnormal electrical pathway, and medications like beta-blockers or calcium channel blockers to control heart rate. Blood thinners are often prescribed to prevent stroke.
What medications are used for atrial fibrillation?
Atrial fibrillation medication can include rate-control drugs (e.g., beta-blockers), rhythm-control drugs (e.g., flecainide, amiodarone), and blood thinners (e.g., apixaban, warfarin) to reduce stroke risk.
Can drugs for atrial flutter and atrial fibrillation be the same?
Often yes – both may use rate-control medications and blood thinners. However, rhythm-control strategies and decisions about procedures like ablation may differ.
How can I tell if I have AFib or atrial flutter at home?
It’s difficult to tell without an ECG. Long term ECG monitoring devices can help detect irregular patterns and assist physicians in detection.
Does atrial flutter always require ablation?
Not always. Some patients are managed with medication first. But ablation is highly effective for atrial flutter treatment, especially when medications don’t work or cause side effects.
Have you ever felt your heart flutter, skip a beat, or suddenly pound for a moment? For many people, this fleeting sensation is caused by something called a Premature Atrial Contraction (PAC) — a common type of irregular heartbeat. While PACs are often harmless, frequent or persistent PACs can sometimes indicate deeper cardiac issues, making awareness and monitoring crucial.
Here, we’ll explore:
- What PACs are
- What do they feel like
- What causes them
- When they may become serious
- How continuous ECG can help
What Are Premature Atrial Contractions (PACs)?
PACs are early heartbeats that originate in the atria, the heart’s upper chambers, before the heart’s natural pacemaker (the sinoatrial node) fires. This disrupts the normal rhythm — often followed by a brief pause — which may feel like a skipped or extra-strong heartbeat.
Real-World Example: When PACs Are More Than Just a Nuisance
In a recent case published in HeartRhythm Case Reports, a 38-year-old woman experienced persistent palpitations due to an unusually high burden of premature atrial contractions (PACs). Despite initial conservative treatment, her symptoms worsened, and imaging revealed impaired left ventricular function. Electrophysiological evaluation confirmed the PACs as the underlying cause. She underwent catheter ablation, after which her heart function and symptoms significantly improved, highlighting that frequent PACs, while often benign, can sometimes lead to reversible cardiomyopathy if left untreated.
This example underscores why it’s essential to understand and track your heart rhythm, especially if symptoms persist.
What Do PACs Feel Like?
PACs can vary in how they’re experienced:
- A fluttering sensation
- A skipped or forceful heartbeat
- Shortness of breath or anxiety
- Or no sensation at all
They’re often more noticeable when lying down or at rest. While many people live with occasional PACs without concern, frequent PACs can signal underlying instability in the heart’s electrical system.
Common Triggers and Risk Factors
PACs may be caused or worsened by:
- Caffeine, alcohol, or nicotine
- Stress, anxiety, or lack of sleep
- Electrolyte imbalances (like low potassium or magnesium)
- Dehydration
- Certain medications
- Underlying heart or lung conditions (like COPD or heart failure)
You’re more likely to experience PACs if you’re older, sedentary, pregnant, have high blood pressure, low HDL (“good”) cholesterol, or live with chronic illness.
When Should You Be Concerned?
PACs are generally benign, but medical evaluation is recommended if:
- They happen frequently or in clusters
- You feel dizzy, faint, fatigued, or have chest discomfort
- You have a history of atrial fibrillation (AFib) or other arrhythmias
- Your quality of life or sleep is affected
High PAC burden (i.e., frequent PACs) is associated with:
- Increased risk of AFib
- Greater likelihood of ischemic stroke
- Progression to heart failure or reduced cardiac output
Diagnosing and Monitoring PACs
PACs are often missed during routine ECGs since they may not occur during a short snapshot. That’s where continuous or ambulatory ECG becomes valuable.
Key Tools Used to Diagnose PACs:
- Electrocardiogram (ECG)
- Holter monitor (24–48 hours)
- Echocardiogram
- Blood tests (to check electrolytes or thyroid function)
But even Holters can miss intermittent Premature Atrial Complexes. For better detection and diagnosis, long-term, wearable ECG devices offer a major advantage.
Why Continuous Monitoring Matters
With continuous ECG-based heart rate monitors, you and your doctor can:
- Catch early signs of arrhythmias
- Track patterns or triggers (like stress or caffeine)
- Reduce anxiety by understanding what’s happening with your heart
- Avoid unnecessary clinic visits through remote medical review
- Make informed decisions about lifestyle changes or treatments
Read more: 24×7 Continuous ECG: The Future of Personalized Heart Health Management
When to Seek Immediate Medical Help
You should seek urgent care if Premature Atrial Complexes are accompanied by:
- Chest pain or pressure
- Persistent shortness of breath
- Fainting or extreme fatigue
- A rapid or irregular heartbeat lasting over 30 minutes
Even if PACs are usually harmless, it’s better to rule out serious conditions early.
Final Thoughts
Premature Atrial Contractions are often a normal part of your heart’s rhythm, but if they become frequent or symptomatic, they deserve attention. With modern continuous ECG monitoring technology, you can take control of your heart health from the comfort of your own home.
Whether you’re investigating palpitations or managing a known arrhythmia, understanding your heart’s rhythm is the first step toward peace of mind and proactive care.
Keywords:
If you take your heart health seriously – whether due to a known condition, family history, or unexplained symptoms – you’ve probably wondered whether a smartwatch is enough to keep tabs on your heart. While smartwatches are great for general wellness, they’re not built for clinical-grade monitoring.
Smartwatches emerged as part of a growing trend towards self-quantification and everyday health awareness. As people sought more control over their fitness, sleep, and heart rate data, tech companies responded with increasingly capable wrist-worn devices that delivered instant feedback. These tools made heart monitoring more accessible to the general public, offering ECG spot checks and irregular rhythm alerts. But despite their innovation, smartwatches were never designed for continuous, medical-grade monitoring. That’s where the Frontier X Plus sets a new standard – giving you and your doctor a much clearer, continuous view of your heart.
In this article, you’ll understand how the Frontier X Plus compares to a typical smartwatch, other available smart watches, and why it’s a better choice if you’re looking for reliable, actionable insights about your heart health.
1. Clinical-Grade ECG vs. Wellness Tracking
Your smartwatch might let you take a 30-60-second ECG reading here and there, usually when you voluntarily remember to check. It may be useful, but not enough if you have symptoms that are intermittent, or if you’re being evaluated for a condition like Atrial Fibrillation.
The Frontier X Plus, however, is an FDA-cleared, prescription device designed for continuous ECG monitoring. You wear it on your chest, and it captures accurate data as you live your life — whether you’re at work, walking the dog, or asleep.
2. Continuous Monitoring That Fits Into Your Life
Unlike a smartwatch, which only records ECGs when you tell it to, Frontier X Plus works in the background, continuously. It records your ECG for up to 24 hours on a single charge, and because it’s designed for daily wear with a quick one-hour recharge, you can use it for days at a time.
If you’ve ever had symptoms that vanish before you could open your watch app, this device is for you.
3. Made for Medical Insight, Not Just Fitness Goals
Smartwatches are great for counting steps and reminding you to stand up, but when it comes to real heart monitoring, they fall short. If your doctor needs to understand your rhythm over time, your smartwatch won’t cut it. The Frontier X Plus is built for exactly that. It’s used in cardiac rehab, post-operative care, and remote patient monitoring, and the data it collects can be reviewed securely by your physician, often without you needing to return to the clinic.
4. Better Accuracy, Less Guesswork
Let’s face it: wrist-based ECGs can be inconsistent. Sweat, movement, or how tight your band is can affect results, sometimes showing false positives or inconclusive data.
The Frontier X Plus sits securely on your chest, providing stable, high-quality ECG signals. If the signal isn’t good, the system flags it, so your doctor only sees clinically reliable data.
5. From Data to Diagnosis, Faster
If your smartwatch tells you something might be off, your next step is usually a referral for further testing. That means waiting, worrying, and possibly wearing a Holter monitor later.
With the Frontier X Plus, you skip the guesswork. Your device collects the data your doctor needs, and a full report, including heart rate trends, arrhythmia flags, and symptom correlations, is generated at the end of your monitoring period.
6. Peace of Mind for People Who Need More Than Alerts
If you’ve been diagnosed with AFib, experience irregular heartbeats, or are just trying to understand concerning symptoms, you deserve better than “maybe” alerts. You deserve clear answers.
The Frontier X Plus gives you confidence that every beat is being tracked, even while you are asleep. That kind of peace of mind simply doesn’t come from a smartwatch.
Read More- Frontier X Plus: The Best Ambulatory ECG Monitor for AFib Detection
The Frontier X Plus vs Smartwatch: At a Glance
| Feature | Frontier X Plus | Smartwatch |
| ECG Type | Continuous, clinical-grade | Intermittent, user-initiated |
| Accuracy | FDA-cleared, validated vs 12-lead ECG | Moderate, lifestyle-grade accuracy |
| Monitoring Duration | 24 hrs per charge, multi-day use | 30–60 sec spot checks |
| Data Access | Cloud dashboard for clinicians | Consumer-facing app only |
| Use Case | Medical-grade monitoring, rehab, IDTFs, extended Holter | Wellness, fitness tracking |
| Comfort | Chest strap, patchless | Wrist-based, less stable for ECG |
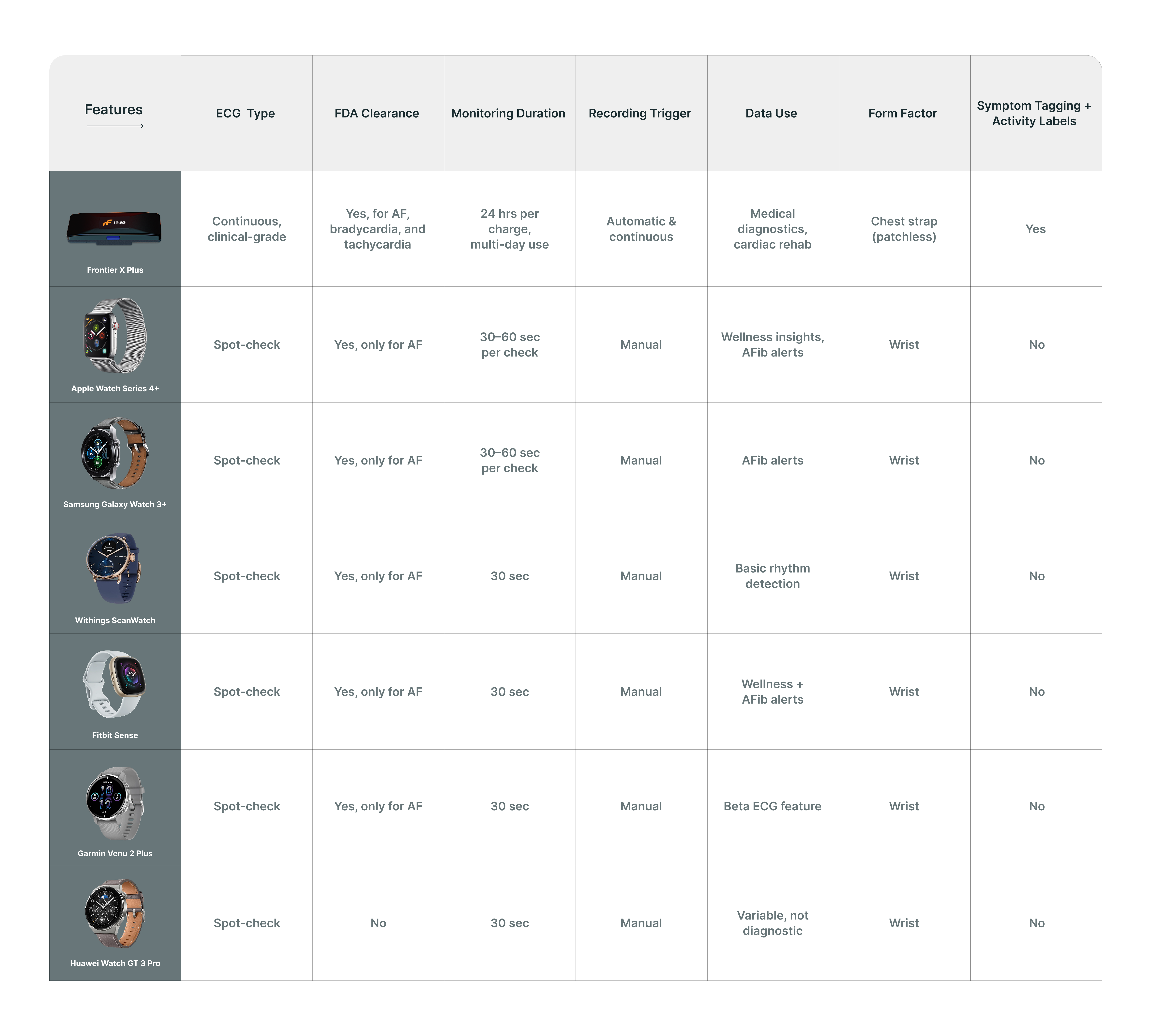
How the Frontier X Plus Compares to Popular Smartwatch Heart Monitors
Final Thoughts
Smartwatches are great wellness companions, but they aren’t made for clinical-level heart monitoring. If your health — or your doctor’s recommendations — demand more than a snapshot, it’s time to consider the Frontier X Plus.
You deserve clarity, accuracy, and continuous insight — and that’s exactly what this device delivers.
To learn more about how the Frontier X Plus supports remote cardiac monitoring, visit Fourth Frontier’s Professional Page.
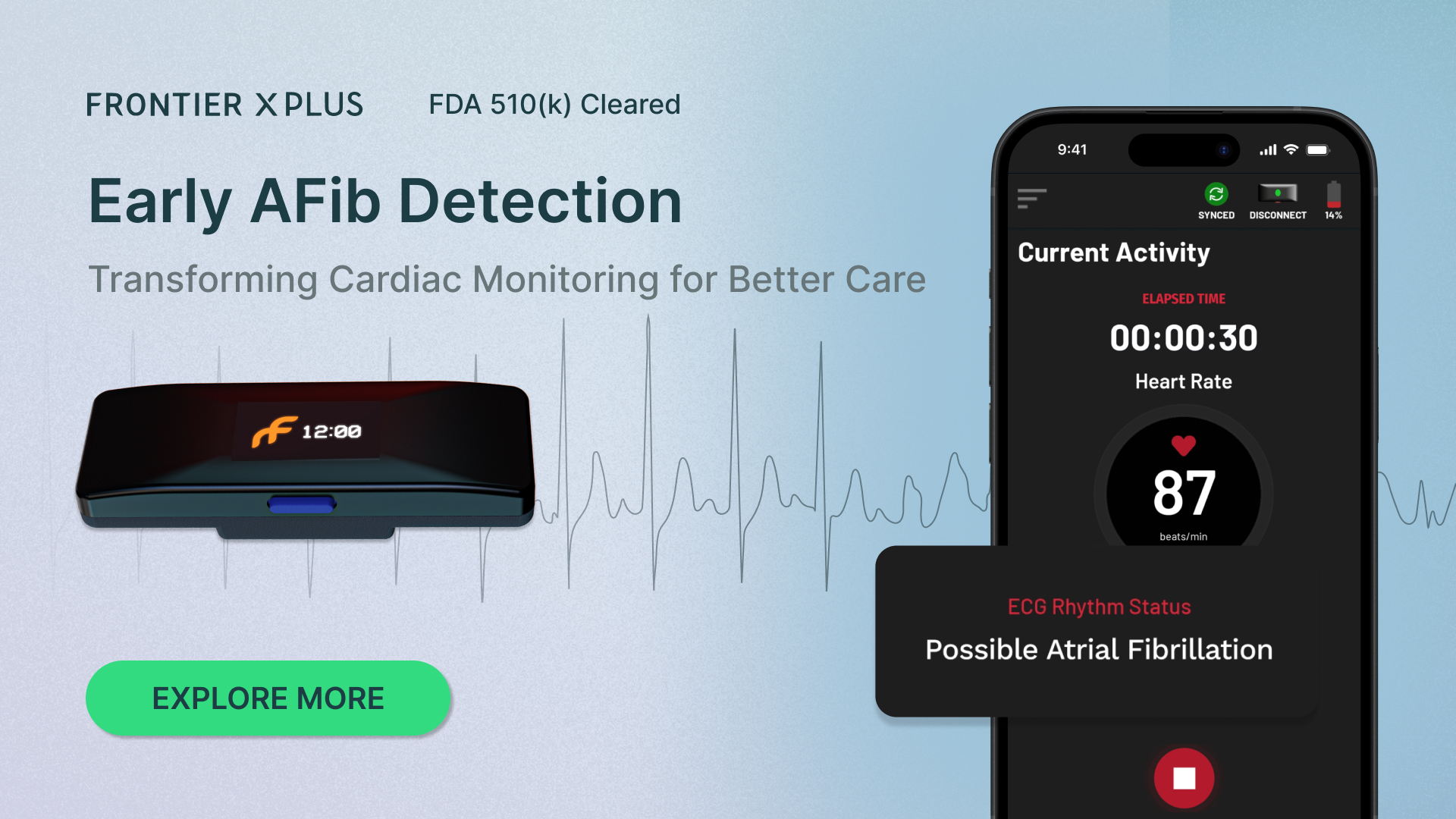
Atrial Fibrillation (AF) is the most common type of arrhythmia affecting millions globally, yet it often goes unnoticed. More than 59 million individuals lived with AF in 2019. Many people live with what’s called asymptomatic AF or silent AF, where irregular heart rhythms occur without any obvious symptoms. While the absence of symptoms might seem like a relief to you, if left unchecked, silent AF raises the risk of serious complications like stroke. That’s where the Frontier X Plus, a patchless continuous ECG monitoring device, comes to your rescue.
Moreover, after your cardiac procedure, monitoring for silent or asymptomatic AF becomes especially important. These irregular heart rhythms, which often occur without symptoms, can significantly increase the risk of stroke if left undetected. Continuous, clinical-grade ECG monitoring with devices like the Frontier X Plus ensures that these hidden episodes are caught early, enabling timely medical intervention during this critical recovery phase.
In this blog, you will explore how the Frontier X Plus enables you and your clinician to detect and manage silent AFs through continuous, real-time, remote heart monitoring — all while you go about your daily routine.
What Is Asymptomatic Atrial Fibrillation/Silent AF?
Asymptomatic AF is when you experience episodes of Atrial Fibrillation without feeling any noticeable symptoms. Unlike typical AF, which can cause palpitations, fatigue, or dizziness, asymptomatic AF may occur silently for months or even years. Yet, it poses the same elevated risks of blood clots, stroke, and heart failure.
According to studies, nearly 27% of AF cases are asymptomatic, and undetected AF is responsible for up to one-third of all strokes. That’s why routine ECG monitoring at home — with a clinically validated device like Frontier X Plus — is essential.
Why Traditional Monitoring Often Falls Short
Standard devices, such as Holter monitors and smartwatches, are not designed to detect intermittent or silent episodes. Holters usually record for only 24–48 hours, which may miss an AFib event entirely, and their bulky design with adhesive electrodes and wires often causes skin irritation and disrupts sleep. Smartwatches, while convenient, rely on short, 30 to 60-second user-initiated ECG recordings and frequently deliver inconclusive or inaccurate results due to poor signal quality or motion. Their wrist-based placement can also lead to signal interruptions during daily movement, reducing reliability for clinical use.
When you’re not feeling symptoms, you likely won’t think of initiating a recording, which is exactly why Frontier X Plus is different.
Read more: Frontier X Plus vs. Holter Monitor: The Future of AFib Detection at Home
The Frontier X Plus: Always-On ECG Monitoring at Home
The Frontier X Plus is an FDA 510(k)-cleared, chest-worn, patchless ECG monitor that captures your heart’s electrical activity continuously throughout the day — even when you’re not aware of anything unusual.
Key features include:
- Continuous ECG monitoring for up to 23 hours per hour of charge, as long as your clinician prescribes, serving as an extended Holter
- Real-time and retrospective ECG data review – Your heart data can be checked both as it’s happening and after the recording is done
- Secure cloud storage accessible by your clinician – Your heart recordings are safely stored online, so your doctor can review them anytime
- Symptom tagging and activity labeling for context – You can note how you’re feeling and what you’re doing during recordings, so your doctor gets the full picture
This makes it ideal for catching asymptomatic AF that may otherwise be missed by short-term or user-activated devices.
Monitoring That Blends Into Your Lifestyle
You don’t need to visit a clinic or stay wired to bulky equipment to take an ECG. With the Frontier X Plus, you simply wear a lightweight, patchless device on your chest using a soft strap. It syncs effortlessly to a companion mobile app, where your data is uploaded to a secure dashboard.
You can go about your routine — working, exercising, sleeping, driving, riding — while your device handles the heart hustle behind the scenes. If something concerning is detected, your physician can review the data and intervene early.
Clinically Actionable Data That Doctors Trust
The Frontier X Plus isn’t just a wellness gadget — it’s a prescription-based tool used in cardiac rehab, remote patient monitoring, and arrhythmia diagnostics. Its advanced algorithms detect:
- Atrial Fibrillation
- Bradycardia
- Tachycardia
- Normal sinus rhythm
At the end of your monitoring period, your doctor receives a detailed report outlining heart rate trends, rhythm breakdowns, and any arrhythmic episodes, giving them the insight they need to make informed treatment decisions.
Peace of Mind Without the Guesswork
Living with asymptomatic AF can feel like living in the dark. The Frontier X Plus shines a light on your heart’s rhythm — even when you don’t feel a thing. Whether you’re being screened for AF due to family history, managing an existing condition, or recovering from a cardiac procedure, this device offers the clarity and confidence you deserve.
Final Thoughts
If you’re at risk of silent arrhythmias like asymptomatic AF, don’t wait for symptoms to appear. With the Frontier X Plus, you get continuous, clinical-grade ECG monitoring — all from the comfort of your own place. Unlike smartwatches or Holters, the Frontier X Plus gives you and your care team the full picture, helping detect AF early and intervene sooner.